Medicaid and Generics: How Generic Drugs Save Money for Low-Income Patients
 Jan, 1 2026
Jan, 1 2026
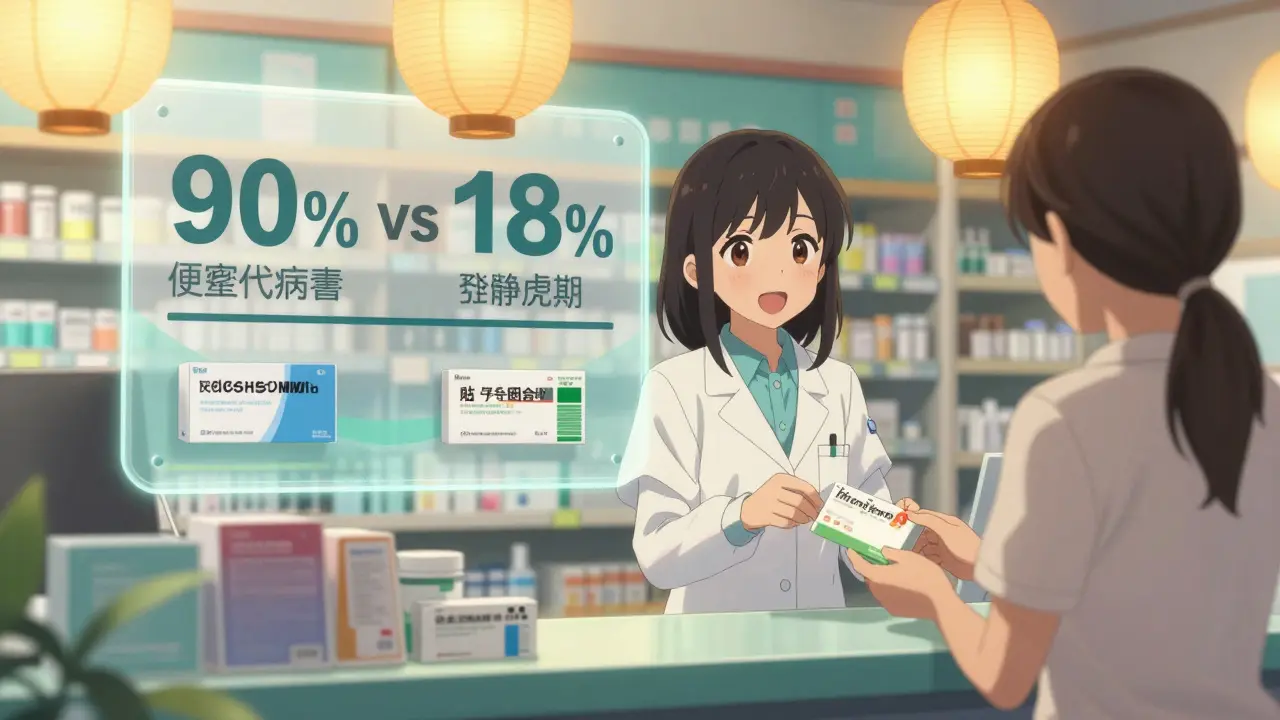
For millions of low-income Americans, Medicaid is the only way they can afford prescription drugs. But here’s the surprising part: generics are the reason most of them can even get their medications at all. In 2023, 90% of all prescriptions filled through Medicaid were for generic drugs. And yet, those same generics made up just 18% of total Medicaid drug spending. That’s not a typo. Generics are saving the program-and the people it serves-billions every year.
Why Generics Are the Backbone of Medicaid
Medicaid doesn’t pay retail prices for drugs. Thanks to the Medicaid Drug Rebate Program (MDRP), the government negotiates deep discounts directly with manufacturers. For generic drugs, those rebates average 86% of the retail price. That means if a generic pill costs $10 at the pharmacy, Medicaid only pays about $1.40 after the rebate. Compare that to brand-name drugs, where rebates are still high but not nearly as steep-around 77% on average. The result? A generic prescription can cost a Medicaid patient $6.16 at the pharmacy counter. A brand-name version? $56.12. Nearly nine times more. This isn’t just about big numbers. It’s about real people. A single mother with diabetes might need insulin, metformin, and blood pressure meds. If those were all brand-name, she’d be paying hundreds a month out of pocket-even with Medicaid. But because those drugs are generic, her total monthly copay is under $20. That’s the difference between taking her medicine and skipping doses.How Much Money Are We Talking About?
In 2023, Medicaid spent $80.6 billion on prescription drugs before rebates. But because of those rebates, the program saved $53.7 billion. That’s more than half of what was spent. Those savings keep Medicaid solvent. Without them, states would have to cut benefits, raise taxes, or turn away patients. The savings ripple outward too. A 2024 report from Stanford Medicine found that between 2009 and 2019, generic drugs saved the U.S. healthcare system $2.2 trillion. That’s not just Medicaid-it’s every program, every insurer, every patient. But Medicaid is where those savings matter most. Low-income patients don’t have savings accounts or credit cards to cover surprise drug costs. Generics keep them alive.Generics vs. Brand-Name: The Real Numbers
Here’s what the data shows when you compare generics and brand-name drugs in Medicaid:| Category | Generic Drugs | Brand-Name Drugs |
|---|---|---|
| Percentage of prescriptions filled | 90-91% | 9-10% |
| Percentage of total drug spending | 17.5-18.2% | 81.8-82.5% |
| Average patient copay | $6.16 | $56.12 |
| Percentage of prescriptions under $20 at pharmacy | 93% | 59% |
| Average rebate from manufacturer | 86% | 77% |
The numbers don’t lie. Generics are the only reason Medicaid can cover so many people. Without them, the program would collapse under the weight of brand-name drug prices.
The Hidden Problem: PBMs and Pharmacy Fees
But here’s the catch: not all the savings make it to the patient. Pharmacy Benefit Managers (PBMs)-middlemen between drug makers, insurers, and pharmacies-take a cut. In Ohio, a 2025 audit found that PBMs collected 31% of the total cost on $208 million worth of generic drugs in just one year. That’s over $64 million in fees. Some of that goes to administrative costs, but a lot of it just disappears into corporate profits. This doesn’t change the fact that generics are still far cheaper than brand-name drugs. But it does mean that even when generic prices drop, patients don’t always see it. Some states have started requiring PBMs to pass savings directly to patients, but most haven’t. That’s why you’ll still hear people say, “My generic cost went down, but my copay didn’t.”Why Specialty Drugs Are Breaking the System
The biggest threat to Medicaid’s cost savings isn’t brand-name drugs-it’s specialty drugs. These are high-cost medications for conditions like cancer, multiple sclerosis, or rare genetic disorders. They’re often biologics-complex molecules that can’t be easily copied like traditional generics. In 2021, drugs costing more than $1,000 per prescription made up less than 2% of all Medicaid claims. But they accounted for over half of total drug spending. That’s the new problem. While 90% of prescriptions are cheap generics, the most expensive 2% are driving up costs faster than ever. Medicaid net spending jumped from $30 billion in 2017 to $60 billion in 2024. That’s a 100% increase in just seven years. The Centers for Medicare & Medicaid Services (CMS) launched the GENEROUS Model in 2024 to tackle this. It’s designed to push states to use better formularies, reduce unnecessary prescriptions, and negotiate better prices on high-cost drugs. But it won’t fix the core issue: we’re running out of affordable alternatives.
What Patients Need to Know
If you’re on Medicaid, here’s what you should remember:- Generics are almost always the cheapest option. Ask your pharmacist to substitute unless your doctor says no.
- Your copay is likely $5-$10 for a 30-day supply. That’s normal. If it’s higher, ask why.
- Some states require prior authorization for certain generics, even if they’re on the formulary. That can delay your refill by days or weeks.
- Don’t assume a brand-name drug is better. Generics have the same active ingredients, same quality standards, and same FDA approval.
- Check your state’s Medicaid website. Each one has its own formulary and rules. Some are easier to navigate than others.
One Medicaid user on Reddit shared that her daughter’s asthma inhaler switched from brand to generic-and her copay dropped from $25 to $3. But it took three weeks of phone calls to get approval. That’s the reality. Generics save money, but the system still gets in the way.
The Future: Biosimilars and Price Negotiation
The next big wave of savings will come from biosimilars. These are cheaper versions of biologic drugs-like insulin or rheumatoid arthritis treatments-that are currently priced like luxury cars. The Association for Accessible Medicines predicts biosimilars could save Medicaid $100 billion annually by 2027. There’s also talk of extending the Inflation Reduction Act’s drug price negotiation rules to Medicaid. Right now, Medicare can negotiate prices for a handful of high-cost drugs. If Medicaid got the same power, experts estimate it could save $15-20 billion over ten years. But none of this matters if we lose sight of the big picture: generics work. They’re safe, effective, and affordable. For low-income patients, they’re not a convenience-they’re a lifeline.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. Generics are not cheaper because they’re lower quality-they’re cheaper because they don’t need to pay for advertising, clinical trials, or patent protection.
Why does my generic drug cost more than last month?
Even though the manufacturer’s price may have dropped, your pharmacy or PBM might not pass that savings on immediately. Some states require pharmacies to notify patients of price changes, but most don’t. If your copay went up, ask the pharmacy for the reason. You may be able to switch to a different generic version or request a price match.
Can I buy generics cheaper outside of Medicaid?
Sometimes. Services like Mark Cuban Cost Plus Drug Company offer lower prices on some generics, but only about 11% of the most common ones. For most Medicaid patients, the program’s negotiated prices are still the best deal-especially when you factor in the rebates and no out-of-pocket costs beyond the small copay. Buying outside Medicaid means losing coverage for other medications and risking gaps in care.
Do all states offer the same generic drug coverage?
No. While federal law requires Medicaid to cover all medically necessary drugs, each state controls its own formulary. Some states have more generics on their list than others. Some require prior authorization for common generics. You can check your state’s Medicaid website or call their pharmacy help line to see which drugs are covered and what rules apply.
Why do some generics have different names?
Generic drugs are named after their active ingredient, not the brand. For example, the generic version of Lipitor is atorvastatin. But different manufacturers may label it as Atorvastatin Calcium, Atorva, or just Atorvastatin. These are all the same drug. Always check the active ingredient on the label, not the brand name on the bottle.

Ann Romine
January 2, 2026 AT 16:07My mom’s on Medicaid and she takes three generics every day. Her copay is $5. If they switched to brand-name, she’d skip doses just to make it last. I’ve seen it happen. Generics aren’t just cheaper-they’re the only thing keeping people alive.
Austin Mac-Anabraba
January 4, 2026 AT 12:41Let’s be precise: the 86% rebate figure is misleading. It’s calculated on the Average Wholesale Price (AWP), a fictional number inflated by manufacturers to create artificial discount margins. The real net price after rebates is often closer to 65-70%. The narrative of ‘generics save billions’ ignores how the system is gamed to make generics look better than they are.
And don’t get me started on PBMs. They’re not middlemen-they’re rent-seekers who extract value without adding utility. The fact that Ohio auditors found $64M in fees on $208M in generics proves the system is broken, not efficient.
Also, ‘same active ingredient’ doesn’t mean same bioavailability. There are documented cases where generic substitutions caused therapeutic failure in epilepsy and psychiatric patients. The FDA’s bioequivalence standards are laughably lax.
Generics aren’t magic. They’re a band-aid on a hemorrhaging system built on price manipulation and regulatory capture.
Phoebe McKenzie
January 5, 2026 AT 08:25Oh please. You’re all acting like generics are some heroic miracle when they’re just the result of corporate greed being masked as public policy. The same companies that make brand-name drugs own the generic versions. They just wait for the patent to expire, then jack up the price on the ‘cheap’ version because they know no one else can compete. That’s not saving money-that’s monopolistic manipulation.
And don’t even get me started on how PBMs and pharmacy chains collude to keep copays high while they pocket the difference. This isn’t about healthcare. It’s about profit. And you people are just cheering for the same wolves in different sheepskins.
My cousin’s insulin generic went from $15 to $45 in six months. And you call that a victory? Wake up.
jaspreet sandhu
January 5, 2026 AT 17:59in india we have generics that cost less than 1 dollar for a month supply of blood pressure medicine. but here in usa people act like it is a miracle that a pill costs 6 dollars. the real problem is not the generics. the real problem is that usa has a broken system where every middleman takes a cut. the drug companies make money. the pbs make money. the pharmacies make money. but the patient still pays too much. why is this so hard to understand? it is not about the pill. it is about the system that eats the savings.
Alex Warden
January 6, 2026 AT 05:29Generics are the reason we’re not bankrupt. If you think we should go back to paying $50 for every pill, you’re either rich or stupid. Medicaid isn’t perfect but it’s the only thing keeping working-class families from choosing between food and insulin. Stop overcomplicating it. Generics save lives. End of story.
LIZETH DE PACHECO
January 6, 2026 AT 08:48My sister just got her first generic prescription after months of fighting for prior auth. Her copay dropped from $28 to $3. She cried. Not because it was cheap-but because she finally didn’t have to choose between paying rent or taking her meds. This isn’t policy. This is survival. Thank you for writing this.
Lee M
January 6, 2026 AT 21:51There’s a deeper truth here: the system doesn’t want you healthy. It wants you dependent. Generics are a temporary fix. The real power lies in who controls the supply chain. Once you understand that PBMs, manufacturers, and insurers are all part of the same machine, you realize the ‘savings’ are just theater. We’re being sold a lie wrapped in a lab coat.
Kristen Russell
January 8, 2026 AT 20:11My dad’s on Medicaid. His generic blood thinner saved his life. He didn’t care if it was branded or not-he just needed it to work. And it did. Sometimes the simplest truth is the most powerful one.
Bryan Anderson
January 10, 2026 AT 06:51Thank you for the thorough breakdown. The data is clear: generics are the backbone of Medicaid’s sustainability. What’s less discussed is the human cost of administrative barriers-prior authorizations, formulary changes, pharmacy network limitations. Even with savings, patients face friction that delays care. The system needs to simplify access, not just reduce price tags. A generic pill is useless if you can’t get it on time.
I’ve worked in community health for 12 years. I’ve seen patients skip doses because the pharmacy didn’t have the generic in stock, or because the prior auth took three weeks. The cost savings mean nothing if the delivery system is broken.
Policy solutions should focus on streamlining prior auth, standardizing formularies across states, and requiring PBM transparency. Generics are the tool. We just need better infrastructure to use it.
Matthew Hekmatniaz
January 10, 2026 AT 20:44My uncle in rural Kentucky gets all his meds through Medicaid. He doesn’t know what a PBM is. He doesn’t care about rebates or formularies. All he knows is that his pills cost $5 and he doesn’t have to choose between them and his grandson’s school supplies. That’s the real win. The numbers are important, but the dignity of being able to take your medicine without fear-that’s what matters.
Let’s not lose sight of that. We’re not just talking about drug costs. We’re talking about people’s ability to live with dignity.
And yes, biosimilars are the next frontier. But let’s fix the broken parts first before we chase the shiny new thing.
Liam George
January 12, 2026 AT 05:54They told us generics were safe. But what if the FDA is compromised? What if the same lobbyists who wrote the patent laws now control the approval process? Think about it-90% of prescriptions are generics, but who owns the patents on the original drugs? Big Pharma. And who manufactures the generics? Big Pharma subsidiaries. This isn’t competition. It’s a shell game. The ‘savings’ are illusions. The real cost is hidden in the quality control gaps, the delayed recalls, the silent deaths from substandard batches. They’re not saving money-they’re sacrificing lives under the guise of efficiency.
And don’t even get me started on the RFID chips they’re embedding in pill bottles. You think that’s for safety? No. It’s for tracking. They’re building a pharmaceutical surveillance state. Wake up.
sharad vyas
January 12, 2026 AT 15:45in india we have a system where generic drugs are produced by thousands of small factories and sold at market prices. no pbs. no corporate middlemen. the price is what the factory charges. the patient pays directly. it works because there is no profit motive between the maker and the user. here in usa the entire system is built on layers of profit. the drug is not expensive because it costs a lot to make. it is expensive because it has to pay for 12 different people to take a cut before it reaches the patient. the solution is not more regulation. the solution is less middlemen.
Paul Ong
January 13, 2026 AT 14:14My cousin got her asthma inhaler switched to generic and her copay dropped from $25 to $3 but it took 3 weeks of calls to get it approved. That’s the real story. The system is broken even when the solution is right in front of us
Bryan Anderson
January 15, 2026 AT 03:49That’s exactly what I was trying to say. The $3 copay is the dream. The three-week wait is the reality. We need to fix the administrative burden, not just the price tag. A system that forces patients to beg for a generic they’re entitled to isn’t saving anything-it’s just shifting the cost to their time, stress, and health.