Latex Allergy: Cross-Reactivity and Workplace Management
 Jan, 3 2026
Jan, 3 2026
Latex allergy isn’t just a nuisance-it can be life-threatening. For some people, touching a rubber glove, a balloon, or even a bandage can trigger a reaction that ranges from itchy skin to full-blown anaphylaxis. What makes this allergy especially tricky is that it doesn’t just come from latex itself. Many people with latex allergy also react to certain foods, and workplaces-especially hospitals-are hotspots for exposure. The good news? This allergy is preventable. The bad news? Once you have it, there’s no cure. The only way to stay safe is to avoid latex completely and know what to do when exposure happens.
What Causes Latex Allergy?
Latex allergy happens when your immune system mistakes proteins from the sap of the Hevea brasiliensis tree as dangerous. These proteins stick to the powder used in older latex gloves, and when the powder becomes airborne, you breathe it in. That’s how many healthcare workers developed allergies in the 1990s-when universal precautions meant everyone wore latex gloves, all day, every day. The powder carried the allergens into the air, and over time, repeated exposure turned harmless contact into a serious immune response.
Not everyone reacts the same way. There are two main types of reactions:
- Type I (immediate): This is IgE-mediated and can be deadly. Symptoms show up within minutes: hives, swelling of the lips or throat, wheezing, drop in blood pressure, and anaphylaxis.
- Type IV (delayed): This is a skin reaction, like contact dermatitis. It shows up 24 to 48 hours later-red, cracked, itchy skin where the latex touched you. It’s not life-threatening, but it’s persistent and annoying.
People with spina bifida are at the highest risk. Why? They often undergo dozens of surgeries as children, and their exposed mucous membranes absorb latex proteins easily. Studies show 20 to 67% of these patients develop latex allergy, and their risk of anaphylaxis during surgery is 500 times higher than average. Even five operations can be enough to trigger it.
Food Cross-Reactivity: The Hidden Danger
One of the most surprising things about latex allergy is how many foods can cause similar reactions. This is called latex-fruit syndrome. The proteins in latex are similar to proteins in certain fruits and vegetables. Your immune system gets confused and attacks both.
Common cross-reactive foods include:
- Bananas
- Avocados
- Kiwi
- Chestnuts
- Potatoes
- Tomatoes
- Apples
- Carrots
Not everyone with latex allergy reacts to all of these. But if you’ve had a strange reaction after eating a banana-swollen lips, itchy throat-you should talk to an allergist. Cross-reactivity isn’t guaranteed, but it’s common enough that doctors now screen for it. The CDC and World Allergy Organization both note that food reactions can be just as severe as those from latex gloves. Some people have had anaphylaxis after eating kiwi, even if they’ve never touched a glove.
Workplace Risks and Who’s Most Affected
Healthcare workers are the most exposed group. Surgeons, nurses, lab techs, and dental staff-anyone who handles gloves daily-are at high risk. Studies show 8 to 12% of healthcare workers are sensitized to latex. That’s three times the rate of the general public.
It’s not just gloves. Latex is in blood pressure cuffs, IV tubing, catheters, tourniquets, and even the seals on some medication vials. In operating rooms, powdered gloves used to be the norm. When the powder floated into the air, it carried allergens into the lungs. Workers developed asthma, runny noses, and eye irritation-sometimes before they even got a rash.
But it’s not just hospitals. Firefighters, hairdressers, cleaners, and even food service workers can be exposed. Latex is in elastic bands, cleaning gloves, and some food handling equipment. The risk rises with time. The longer you work in a high-exposure job, the higher your chance of developing an allergy.

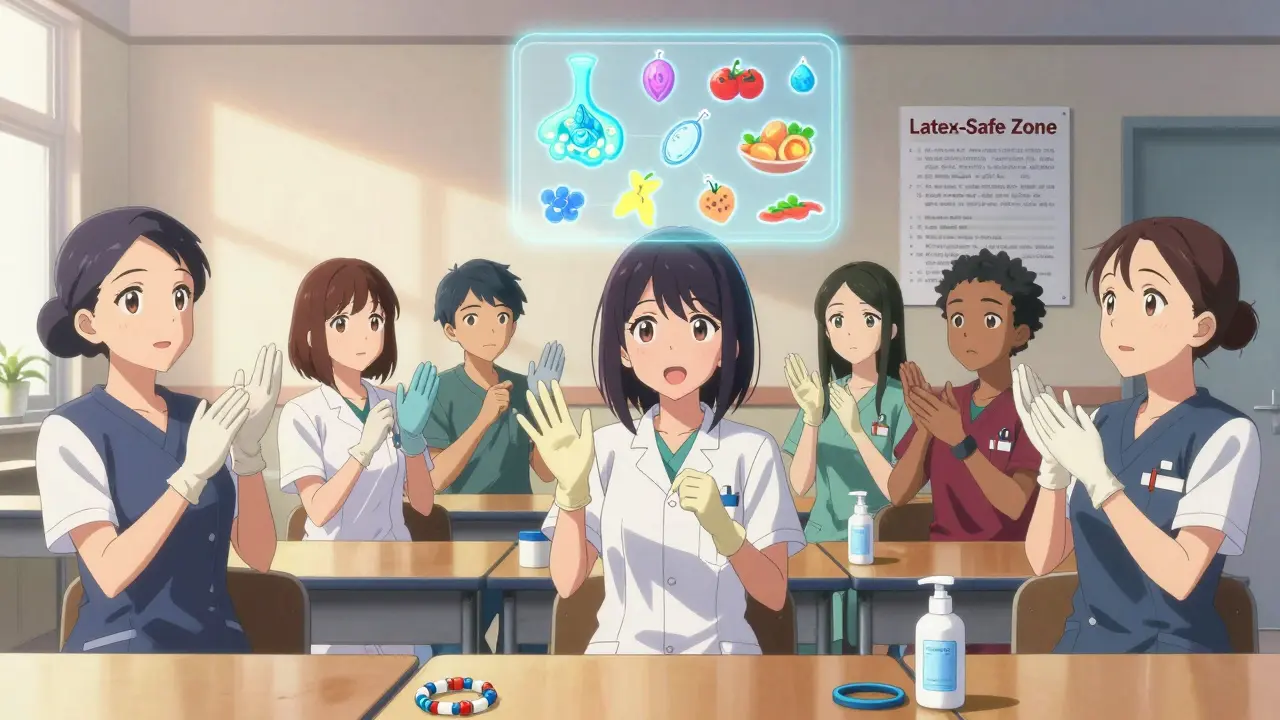
How Workplaces Can Protect Employees
The solution isn’t to stop using gloves. It’s to stop using latex gloves.
Germany banned powdered latex gloves in the late 1990s. Within a few years, new cases of latex allergy among healthcare workers dropped by nearly 80%. Finland saw the same drop. These countries didn’t just switch gloves-they changed policy, trained staff, and monitored compliance.
Here’s what works:
- Replace powdered latex gloves with non-powdered nitrile, neoprene, or vinyl gloves. Modern synthetics are just as durable and often more comfortable.
- Label all latex-containing products clearly. If a blood pressure cuff has latex, it should say so.
- Create a latex-safe zone in high-risk areas like operating rooms. Only non-latex products allowed.
- Train staff on cross-reactivity, symptoms, and emergency response.
- Establish a latex advisory committee that reviews all purchasing decisions. No more hidden latex in new equipment.
Hand hygiene matters too. Dry, cracked skin from frequent washing makes it easier for allergens to enter the body. Using moisturizers designed for sensitive skin reduces risk.
What Individuals With Latex Allergy Must Do
If you’ve been diagnosed with latex allergy, your life changes-but it doesn’t have to be limited. Here’s what you need to do:
- Carry an epinephrine auto-injector at all times. If you’ve ever had a severe reaction, this isn’t optional. Epinephrine is the only thing that can stop anaphylaxis in minutes.
- Wear a medical alert bracelet. In an emergency, you might not be able to speak. A bracelet tells paramedics to avoid latex.
- Make an Anaphylaxis Action Plan with your doctor. Know the steps to take if you react-when to use epinephrine, when to call 911.
- Inform everyone. Dentists, doctors, employers, teachers, even friends who host dinner parties. Latex is in balloons, party favors, and some condoms. Don’t assume they know.
- Check everyday items. Replace rubber bands with silicone ones. Use vinyl or silicone shower mats. Choose synthetic rubber soles on shoes. Avoid latex mattresses and pillows.
Don’t rely on “hypoallergenic” labels. That term isn’t regulated. A product labeled hypoallergenic might still contain latex. Always read the ingredient list or ask the manufacturer.
Treatment and Emergency Response
There’s no cure. No shots. No pills that make you immune. The only treatment is avoidance. But if you do react, here’s what to do:
- Anaphylaxis: Use epinephrine immediately. Don’t wait. Call emergency services. Lie down with legs elevated. Even if you feel better after the shot, you still need to go to the hospital. A second wave of symptoms can happen hours later.
- Mild skin reaction: Wash the area with soap and water. Apply 1% hydrocortisone cream. Take an oral antihistamine if needed.
- Respiratory symptoms: Wheezing, chest tightness, trouble breathing? Use your epinephrine. Call 911. Don’t try to “wait it out.”
Antihistamines and steroids help with mild symptoms, but they do nothing for anaphylaxis. Only epinephrine saves lives here.
The Future of Latex Allergy Management
Manufacturers have made big improvements. Many latex gloves now go through chlorination, which reduces allergen levels. Powder-free gloves are standard in most hospitals. New synthetic materials are stronger, more flexible, and cheaper than ever.
Research is looking at recombinant latex allergens for better diagnosis. Maybe one day, immunotherapy will help desensitize people-but right now, that’s still experimental. Until then, avoidance is the gold standard.
The message is clear: latex allergy is preventable. It’s not something you have to live with if workplaces do their part. And if you’re allergic, you can live a full, safe life-if you’re informed, prepared, and never stop asking, “Is this latex?”
Can you outgrow a latex allergy?
No, latex allergy is not something you outgrow. Once your immune system becomes sensitized, the reaction can last a lifetime. Avoidance is the only way to prevent symptoms. Even if you haven’t had a reaction in years, exposure can trigger it again.
Are all latex gloves dangerous?
Not all gloves are the same, but if you’re allergic to natural rubber latex, any glove made from it-even powder-free-is risky. The allergens are in the protein, not the powder. Always choose synthetic alternatives like nitrile, vinyl, or neoprene. Look for labels that say “latex-free” and avoid products labeled “natural rubber” or “rubber.”
Can I use latex-free gloves if I’m not allergic?
Yes, and you should-especially in workplaces where someone else might be allergic. Even if you’re not sensitive, powdered latex gloves can spread allergens through the air. Switching to non-latex gloves protects everyone. Many hospitals now use nitrile gloves as standard, not just for allergic staff but for all employees.
Do all foods that cross-react with latex cause reactions?
No. Cross-reactivity varies from person to person. Some react to bananas but not avocados. Others react to chestnuts but not kiwi. There’s no universal list. The best approach is to keep a food diary after eating potential cross-reactive foods. If you notice symptoms like itching in the mouth or throat, talk to your allergist. They can do skin or blood tests to confirm triggers.
Is latex allergy more common in certain countries?
Yes. Countries with high healthcare glove usage and older glove policies had higher rates-like the U.S. in the 1990s. After Germany and Finland banned powdered latex gloves, new cases dropped sharply. Today, countries with strict workplace regulations have lower rates. But in places where synthetic gloves are expensive or hard to get, latex allergy remains a bigger problem.

Jacob Milano
January 4, 2026 AT 17:35Man, I never realized how many everyday things contain latex until I read this. Rubber bands? Shower mats? Shoe soles? I just replaced all mine with silicone. Feels like I just unlocked a secret level of safety. Also, now I know why my cousin broke out in hives after eating a banana at a picnic-no one even thought to ask if she had allergies. This post is a game-changer.
Dee Humprey
January 5, 2026 AT 15:42Carrying epinephrine isn’t optional. Period. 🩺 I’ve seen someone go down in under 90 seconds. If you’re allergic, get the script. Wear the bracelet. Tell your boss. Don’t wait for a near-death experience to take it seriously. This isn’t drama-it’s survival.
Aaron Mercado
January 6, 2026 AT 02:23Wait-so we’re just supposed to trust that ‘latex-free’ labels are accurate?!!?? That’s a joke, right?!! Companies lie about ingredients ALL THE TIME! I bet the FDA’s asleep at the wheel again… and don’t get me started on how hospitals still use ‘hypoallergenic’ as a marketing gimmick while hiding latex in IV tubing!! This is corporate negligence!!
saurabh singh
January 7, 2026 AT 02:11Bro, this hits different in India. We use latex gloves everywhere-hospitals, street food stalls, even barber shops. No one thinks twice. But I’ve seen my cousin break out in rashes after handling mangoes. Turns out, he’s allergic to latex AND mangoes. We’re way behind on awareness here. Need to push for training in local clinics. This info? Gold.
John Wilmerding
January 8, 2026 AT 17:39While the article provides a comprehensive overview of latex allergy and its implications, I would like to underscore the importance of standardized workplace protocols. The transition from powdered latex to synthetic alternatives is not merely a matter of preference-it is a public health imperative. Institutions must adopt enforceable policies, not merely recommendations.
Stephen Craig
January 10, 2026 AT 15:16It’s funny how something so small-a tree’s sap-can control so much of our lives. We fear the invisible. The protein. The powder. The banana. The glove. We build walls around ourselves to avoid it. But maybe the real problem isn’t the latex… it’s that we never learned to ask ‘what else is hiding here?’
Clint Moser
January 11, 2026 AT 11:52They say latex allergy is preventable… but who’s really behind the scenes pushing for nitrile? Big Pharma? The glove conglomerates? I’ve seen the patents-latex-free gloves cost 3x more to produce. So why are they pushing this ‘safe alternative’ narrative? Coincidence that the same companies own the patents on epinephrine auto-injectors? Hmmmm…
Enrique González
January 11, 2026 AT 13:29My sister’s a nurse. She got diagnosed after three years of skin rashes. She switched to nitrile, started using moisturizer religiously, and now she’s fine. But no one in her hospital told her about the food stuff. She ate kiwi at brunch last month and thought she was having a cold. Turns out-latex cross-reactivity. She’s lucky she didn’t collapse. This needs to be taught in med school.
bob bob
January 12, 2026 AT 20:41Just had my first anaphylaxis scare last year after a dental visit. They didn’t even ask if I was allergic. I had to tell them. Now I carry two epinephrine pens. And I ask EVERYONE. ‘Is this latex?’ Even my barista. She laughed. Then she cried. Turns out her mom died from it. We need more of these conversations.
Joseph Snow
January 12, 2026 AT 22:31Latex allergy? More like a manufactured crisis. The real issue is overdiagnosis. People panic over a rash and label themselves allergic. Then they demand special treatment. Hospitals are drowning in liability lawsuits because of this. The data is inflated. Stop fearmongering.
Roshan Aryal
January 13, 2026 AT 05:46USA thinks it’s the center of the world. But in India, we use natural rubber gloves because they’re cheap. Your ‘latex-free’ fancy gloves? Unaffordable for 80% of clinics here. So don’t come preaching about ‘safe zones’ when people are choosing between gloves and food. This isn’t a privilege-it’s a class issue.
Angie Rehe
January 14, 2026 AT 14:13Okay but did you know that some latex-free gloves still contain trace proteins from manufacturing? I’ve got lab data. The FDA doesn’t test for it. And guess what? They’re still using powdered nitrile in some hospitals. It’s a cover-up. I’ve filed 3 FOIA requests. No one’s talking about this. I’m not paranoid-I’m just the only one with the files.
mark etang
January 15, 2026 AT 18:09While the article presents a compelling case for workplace reform, it is imperative to note that the economic burden of transitioning to synthetic alternatives must be addressed through federal subsidies and tax incentives. Without institutional support, compliance remains inconsistent.
Jack Wernet
January 17, 2026 AT 14:54I appreciate the depth of this post. As someone who works in occupational health, I’ve seen firsthand how latex exposure affects workers over time. The real tragedy isn’t the allergy-it’s how long it takes for institutions to act. We need mandatory training, not just guidelines. And we need to protect the vulnerable-not just the loud ones.