How Viral Hepatitis Triggers Hepatic Encephalopathy: Pathways & Management
 Sep, 24 2025
Sep, 24 2025
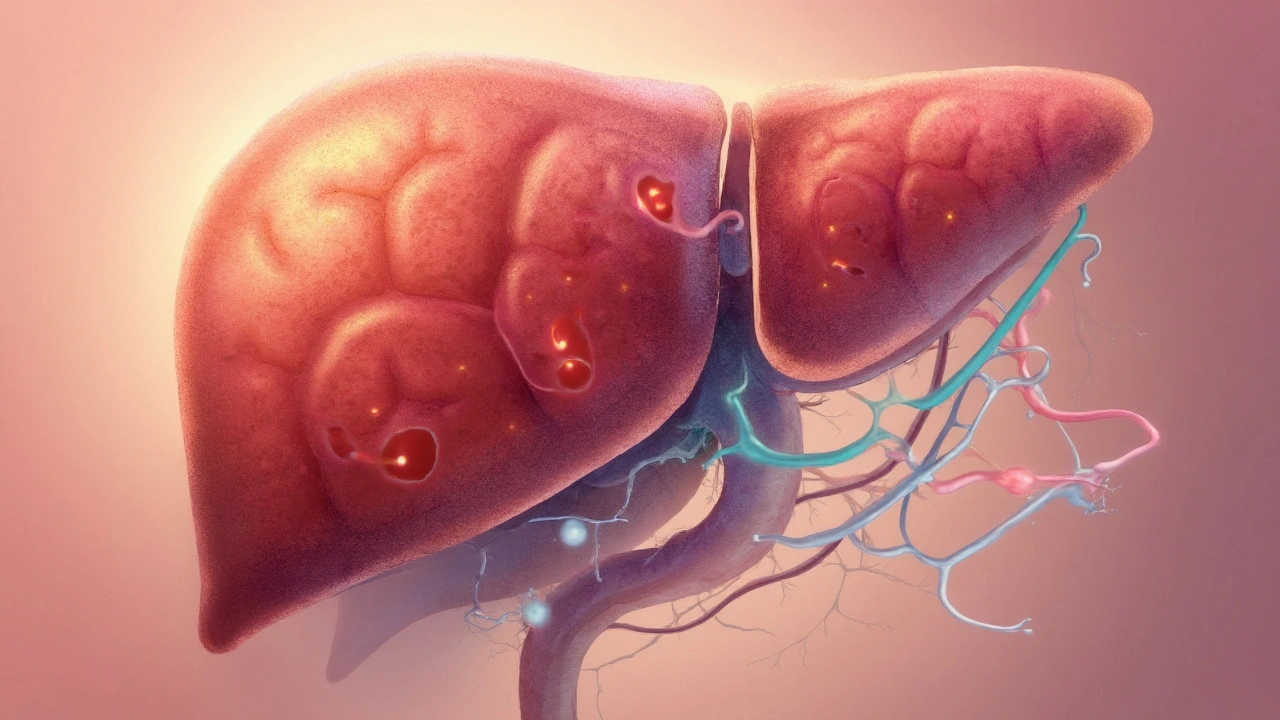
Hepatic Encephalopathy is a neuropsychiatric syndrome that arises when the liver can no longer detoxify harmful substances, especially ammonia, leading to brain dysfunction. While many associate it with alcohol‑related liver disease, a sizable share of cases stems from viral hepatitis chronic infections of the liver caused primarily by hepatitis B virus (HBV) and hepatitis C virus (HCV). Understanding the link helps clinicians catch early warning signs, and patients can take steps to lower their risk.
Quick Take
- Chronic HBV or HCV can progress to cirrhosis, the main gateway to hepatic encephalopathy.
- Elevated serum ammonia, neuroinflammation, and portal‑systemic shunting are the key pathophysiologic bridges.
- Lactulose and rifaximin remain first‑line treatments, while liver transplantation offers a cure for end‑stage disease.
Why Viral Hepatitis Matters for Brain Health
Both HBV and HCV infect liver cells and trigger persistent inflammation. Over years, this inflammation stimulates fibrosis, eventually reshaping normal liver architecture into liver cirrhosis a stage where scar tissue replaces healthy tissue, impairing detoxification. Cirrhosis reduces the liver’s ability to convert ammonia-produced by gut bacteria from protein-to urea, which the kidneys can safely excrete. When ammonia accumulates, it crosses the blood‑brain barrier, disrupting neurotransmission and causing the cognitive & motor abnormalities that define hepatic encephalopathy.
Key Players in the Hepatitis‑HE Cascade
The cascade involves several interconnected entities. Below is a snapshot of the most consequential ones:
- Ammonia a neurotoxic by‑product of protein metabolism that the liver normally converts to urea
- Portal‑systemic shunt abnormal vascular routes that bypass the liver, allowing toxins to reach systemic circulation
- Neuroinflammation activation of brain microglia by circulating toxins, amplifying neuronal dysfunction
- MELD score Model for End‑Stage Liver Disease, a numeric predictor of mortality used to prioritize transplant candidates
- Child‑Pugh classification a scoring system that grades cirrhosis severity based on bilirubin, albumin, INR, ascites, and encephalopathy
Comparing Hepatitis B and C: How Each Drives Encephalopathy
| Virus | Typical Chronicity | Progression to Cirrhosis (Years) | Reported HE Incidence |
|---|---|---|---|
| HBV | 20‑30% become chronic | 15‑20 | ≈10% of cirrhotic HBV patients |
| HCV | ≈75‑85% chronic after infection | 10‑15 | ≈20‑30% of cirrhotic HCV patients |
Both viruses push the liver toward fibrosis, but HCV tends to produce cirrhosis faster and more often, translating into a higher observable rate of hepatic encephalopathy. The difference matters when clinicians decide how aggressively to screen for early neurocognitive changes.

Detecting Early Encephalopathy in Hepatitis Patients
Screening hinges on a blend of clinical observation, lab values, and simple bedside tests.
- **Clinical grading** - Use the West Haven criteria (grades 0‑4) to classify mental status.
- **Serum ammonia** - Though not perfectly specific, levels >80µmol/L often signal overt HE.
- **Psychometric hepatic encephalopathy score (PHES)** - A series of paper‑pencil tasks that catch subtle deficits.
- **Neuroimaging** - MRI may reveal hyperintensities in the basal ganglia linked to chronic ammonia exposure.
Patients with chronic HBV or HCV should undergo HE screening at the time cirrhosis is diagnosed (Child‑Pugh B or higher) and whenever they present with new confusion, asterixis, or sleep‑wake cycle disturbances.
Therapeutic Strategies: From Toxins to Transplant
Management falls into three tiers: reducing ammonia production, increasing ammonia removal, and addressing the underlying liver disease.
- Lactulose a synthetic disaccharide that acidifies the colon, converting ammonia (NH₃) to non‑absorbable ammonium (NH₄⁺). Doses start at 25mL orally three times daily and are titrated to 2‑3 soft stools per day.
- Rifaximin a non‑systemic antibiotic that suppresses ammonia‑producing gut bacteria. Standard regimen: 550mg twice daily, often added when lactulose alone fails.
- **Nutritional adjustments** - Moderate protein (1.2‑1.5g/kg) maintains muscle mass while avoiding excessive catabolism that would raise ammonia.
- **Antiviral therapy** - Direct‑acting antivirals (DAAs) for HCV and tenofovir/entecavir for HBV can halt disease progression, indirectly reducing HE risk.
- **Liver transplantation** - For refractory HE (≥grade3) with MELD ≥15, transplantation offers definitive cure. Post‑transplant survival exceeds 85% at five years.
Choosing the right mix depends on HE severity, patient comorbidities, and the stage of viral hepatitis. A collaborative approach between hepatology, infectious disease, and nutrition teams yields the best outcomes.
Practical Checklist for Clinicians
- Identify chronic HBV/HCV patients with cirrhosis (Child‑Pugh B or higher).
- Order baseline serum ammonia and PHES at diagnosis.
- Start lactulose promptly; add rifaximin if ammonia remains >80µmol/L after 5days.
- Initiate or continue antiviral therapy per current AASLD guidelines.
- Re‑evaluate MELD and Child‑Pugh scores quarterly; refer for transplant evaluation when MELD ≥15 or HE becomes refractory.
Related Concepts Worth Exploring
Understanding hepatic encephalopathy opens doors to several adjacent topics that readers often find useful:
- **Portal hypertension** - The pressure rise that fuels shunt formation.
- **Ascites management** - Fluid accumulation that can exacerbate HE.
- **Co‑infection dynamics** - How HIV or HDV co‑infection modifies hepatitis progression.
- **Non‑alcoholic fatty liver disease (NAFLD)** - Another major driver of cirrhosis and HE in the modern era.
Future articles could dive deeper into each of these, linking back to the core theme of liver‑brain interaction.

Frequently Asked Questions
Can viral hepatitis cause hepatic encephalopathy without cirrhosis?
Rarely. Most cases require at least moderate fibrosis because the liver’s detox capacity must be substantially compromised. Isolated HE in early hepatitis is usually a red flag for an undiagnosed shunt or another metabolic disorder.
How fast does hepatitis C lead to hepatic encephalopathy?
On average, chronic HCV progresses to cirrhosis in 10‑15years, and once cirrhosis is established, overt HE can appear within a few months to 2years, especially if precipitating factors like infections or renal dysfunction arise.
Is lactulose safe for patients with renal failure?
Lactulose itself is not nephrotoxic, but the resulting electrolyte shifts (especially potassium loss) can be problematic. Dose adjustments and close monitoring of serum electrolytes are advised.
Do direct‑acting antivirals reduce the risk of hepatic encephalopathy?
Yes. By achieving sustained virologic response (SVR) in >95% of treated patients, DAAs halt ongoing inflammation and can even lead to regression of fibrosis, lowering the chance of future HE episodes.
What lifestyle changes help prevent hepatic encephalopathy?
Maintain a balanced protein intake, avoid alcohol, stay hydrated, chew food thoroughly, and manage constipation. Regular monitoring of liver function and adherence to antiviral regimens are equally vital.

Hamza Asghar
September 25, 2025 AT 20:44Let’s be real - if you’re still using Child-Pugh over MELD in 2025, you’re practicing hepatology like it’s 2008. The whole 'ammonia = bad' narrative is outdated. We’ve known for years that neuroinflammation and GABAergic dysregulation are the real culprits. Ammonia’s just the visible smoke, not the fire. And don’t get me started on lactulose - it’s basically sugar water with side effects. Rifaximin’s the only thing that actually changes outcomes, and even then, only if the patient isn’t already in grade 3 encephalopathy. Stop treating labs and start treating brains.
Karla Luis
September 26, 2025 AT 00:24Actually i’ve seen patients with hcv cirrhosis and normal ammonia but still grade 2 he. The phes score picked it up before anyone noticed they were forgetting their grandkids’ names. Ammonia’s just one piece. Also lactulose makes people bloated as hell and then they stop taking it. Rifaximin’s cheaper than hospital stays tbh. And yes i know this is basic but if you’re not checking for constipation in these patients you’re doing it wrong. Just saying.
jon sanctus
September 26, 2025 AT 12:13OMG I just had a patient with HCV cirrhosis who developed HE after a weekend of binge drinking and antibiotics - she was in a coma for 72 hours. I thought I was prepared until I saw her pupils dilate and her hands flapping like she was conducting an orchestra of death. Lactulose didn’t help. Rifaximin barely helped. We had to intubate her. And then her husband asked if she could still watch Netflix. I cried in the supply closet. This isn’t medicine. This is torture with a clipboard. Also - antivirals are miracles. If your patient has HCV and you’re not treating it, you’re basically signing their brain death warrant.
Kenneth Narvaez
September 27, 2025 AT 16:03Portal-systemic shunting is the primary pathophysiologic driver of ammonia bypass. The hepatic clearance capacity is reduced due to parenchymal loss and vascular remodeling. Lactulose induces colonic acidification, shifting NH3 to NH4+, which is non-diffusible. Rifaximin modulates gut microbiota composition, reducing urease-producing species such as Klebsiella and Proteus. DAAs achieve SVR in >95% of cases, leading to histological improvement in fibrosis stage, which correlates with reduced HE incidence. MELD score >15 indicates transplant candidacy. PHES is more sensitive than clinical grading for minimal HE. No emoticons. No fluff. Just data.
Christian Mutti
September 27, 2025 AT 18:05As a clinician who has witnessed the slow, silent erosion of cognition in patients with chronic viral hepatitis - I can say with absolute certainty that this is one of the most underappreciated tragedies in modern hepatology. We screen for cancer, we monitor for fibrosis, we obsess over viral loads - but when a patient starts forgetting their own name? We call it ‘encephalopathy’ like it’s a footnote. It’s not. It’s the soul leaving the body, one ammonia molecule at a time. And yes - transplantation saves lives. But it doesn’t bring back the years lost to confusion, to silence, to the quiet shame of being a burden. We need to treat the brain like it matters. Not just the liver.