Complete Guide to Over-the-Counter Medications for Safe Self-Care
 Dec, 5 2025
Dec, 5 2025
Every year, millions of people reach for an OTC medication to treat a headache, a cold, or an upset stomach. It’s quick. It’s easy. And most of the time, it works. But here’s the truth most people don’t talk about: OTC medications aren’t harmless. They can hurt you if you don’t know what you’re doing.
You might think, ‘It’s just a pill from the shelf-how dangerous could it be?’ But acetaminophen alone sends over 56,000 people to the emergency room every year in the U.S. because someone took too much. Ibuprofen causes 103,000 hospitalizations from stomach bleeding. And how many of us actually read the label? Only 22% do. The rest guess. Wing it. Assume. That’s where things go wrong.
What Exactly Counts as an OTC Medication?
When you think OTC, you probably picture painkillers or cough syrup. But OTC includes a lot more. Fluoride toothpaste? That’s an OTC drug. Antifungal dandruff shampoo? OTC. Eye drops for redness? OTC. Even some first-aid creams with antibiotics count. The FDA regulates over 800 active ingredients in more than 100,000 OTC products. That’s not just pills-it’s an entire ecosystem of self-care tools.
These aren’t random products. They’ve been reviewed for safety and effectiveness. The FDA’s OTC Drug Review, started in 1972, set the rules. And in 2020, the CARES Act updated the system to move faster on safety fixes. That means the products on your shelf today are better regulated than ever. But that doesn’t mean they’re foolproof.
The Big Four: Pain Relief Medications
Two drugs dominate the pain relief market: acetaminophen and ibuprofen. They’re everywhere. But they’re not interchangeable.
Acetaminophen (Tylenol, Paracetamol) is your go-to for headaches, fever, or mild aches. It doesn’t reduce swelling like NSAIDs do, but it’s gentler on the stomach. The catch? Your liver can’t handle more than 3,000 mg in a day. That’s six extra-strength tablets. If you’re also taking a cold medicine with acetaminophen? You’re doubling up. And that’s how liver damage happens.
Ibuprofen (Advil, Motrin) is better for inflammation-sprains, arthritis, menstrual cramps. It works by blocking enzymes that cause swelling and pain. But it’s harder on your gut. If you have a history of ulcers, high blood pressure, asthma, or are on blood thinners, this isn’t safe for you. And here’s the kicker: long-term use-even at OTC doses-can raise your risk of heart attack or stroke. Since April 2023, every NSAID label in the U.S. must warn about this.
Naproxen sodium (Aleve) is another NSAID, but it lasts longer. One tablet can give you 12 hours of relief. But the daily max is only 660 mg. That’s just three pills. Many people think, ‘It’s OTC, so I can take more.’ Don’t.
What’s in the Rest of the Shelf?
OTC meds aren’t just about pain. Here’s what else you might be using-and what to watch for.
- Heartburn and indigestion: Bismuth subsalicylate (Pepto-Bismol) works for nausea and diarrhea. But it contains salicylate, the same compound as aspirin. If you’re allergic to aspirin or take blood thinners, skip it. Antacids like calcium carbonate (Tums) are safer for occasional use, but overuse can cause kidney stones or electrolyte imbalances.
- Cough and cold: Guaifenesin (Mucinex) thins mucus. Dextromethorphan suppresses coughs. But many cold formulas combine these with decongestants like pseudoephedrine or antihistamines like diphenhydramine. The problem? You might not realize you’re taking multiple drugs with the same active ingredient. A Reddit user shared how they bought a nighttime cold medicine thinking it was just for sleep-only to find out it had diphenhydramine, which left them groggy all day. That’s why single-ingredient products are often safer.
- Allergy relief: Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are non-drowsy options. Diphenhydramine (Benadryl) works fast but knocks you out. Use it only for short-term relief.
- Topical treatments: Hydrocortisone cream for rashes, salicylic acid for warts, and antifungal sprays for athlete’s foot are all OTC. But don’t use hydrocortisone on your face unless directed. Don’t use wart removers on moles. Don’t apply antifungals for more than four weeks without seeing a doctor.
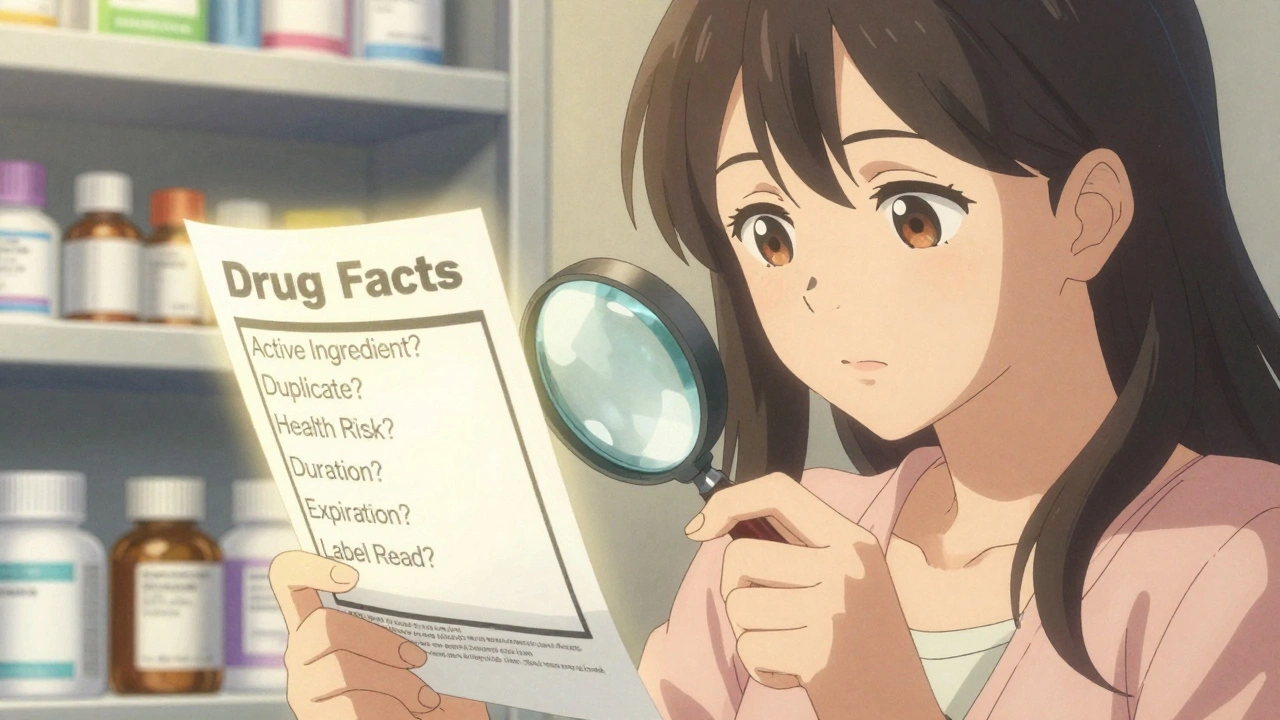
The Drug Facts Label: Your Secret Weapon
Every OTC medicine sold in the U.S. must have a Drug Facts label. It’s not just a design-it’s a legal requirement. And it’s the only thing standing between you and a bad decision.
Here’s what you need to check every single time:
- Active ingredients: This is the medicine itself. Know what’s in it. If you’re already taking another drug with the same ingredient, you’re overdosing.
- Purpose: What is this for? If your symptom isn’t listed, don’t take it.
- Uses: Specific conditions it treats. Not ‘for pain’-but ‘for minor aches and pains due to cold, flu, or headache’.
- Warnings: Who shouldn’t take it? What to avoid? This section is where the real danger lies.
- Directions: How much? How often? For how long? Never exceed the daily max.
- Inactive ingredients: These are fillers, dyes, flavors. If you’re allergic to dyes or gluten, check here.
Most people skip to the ‘Directions’ and stop. That’s like reading only the last page of a recipe. You need the whole thing.
Who’s at Risk? And Why?
OTC misuse isn’t just about being careless. It’s often about confusion, lack of information, or thinking ‘it’s harmless.’
Older adults are the most vulnerable. Nearly 24% of people over 65 take five or more prescription drugs. Adding an OTC painkiller or sleep aid can create dangerous interactions. One study found that 6.7% of adverse drug events in seniors come from OTC meds.
People with low health literacy struggle with labels. Only 12% of U.S. adults have proficient health literacy. That means most can’t understand ‘take every 6 hours as needed’ or ‘do not exceed 6 tablets in 24 hours.’ They might think ‘as needed’ means ‘whenever I feel like it.’
Parents make the most common mistake: dosing children’s liquid acetaminophen wrong. The concentration changed in 2011 to reduce overdoses-but many still use old spoons or kitchen teaspoons. A teaspoon isn’t 5 mL. A dosing cup is. Always use the one that comes with the bottle.
People with chronic conditions often assume OTC meds won’t interfere. But ibuprofen can raise blood pressure. Decongestants can spike heart rate. Antacids can mess with kidney function. If you have diabetes, heart disease, kidney issues, or liver disease-ask a pharmacist before taking anything.
When Should You See a Doctor Instead?
OTC meds are for short-term relief. Not long-term fixes. Here’s when to stop self-treating and call a doctor:
- Pain lasts more than 10 days
- Fever stays above 102°F for more than 3 days
- Cough lasts longer than 2 weeks
- Stomach pain gets worse or spreads
- You notice black, tarry stools (sign of internal bleeding)
- You develop a rash after taking a new OTC med
- You feel dizzy, confused, or have trouble breathing
If you’re not sure, wait 48 hours. If symptoms don’t improve-or get worse-see someone. OTC meds mask symptoms. They don’t cure the cause.
How to Use OTC Medications Safely
Here’s a simple three-step system that cuts your risk of error by 68%, according to the American Society of Health-System Pharmacists:
- Match symptoms to the label. Don’t assume. Read the ‘Uses’ section. If your symptom isn’t listed, don’t take it.
- Check for duplicate ingredients. Open your medicine cabinet. Look at every pill, syrup, or patch you’re taking. If two have the same active ingredient, you’re doubling up. That’s how overdoses happen.
- Verify your dose. Age, weight, and health conditions change what’s safe. A 120-pound woman and a 200-pound man need different doses. Kids need weight-based dosing. Never use adult doses for children.
Also: write down what you take. Keep a list. Update it every time you start or stop something. Bring it to your doctor or pharmacist. They’ll catch things you miss.

Pharmacists Are Your Best Resource
Most people think pharmacists just hand out pills. But 78% of pharmacists provide OTC counseling every year. They check for interactions. They spot duplicate ingredients. They explain labels in plain language.
And it works. Pharmacies offering free medication reviews have seen a 42% drop in inappropriate OTC use. Yet only 22% of people ask for help. Why? Because they don’t think they need to. Or they’re embarrassed. Or they assume it’s free advice is ‘just sales.’
It’s not. Pharmacists are trained to keep you safe. Walk up to the counter. Say, ‘I’m thinking of taking this for my headache. Is it safe with what I’m already on?’ They won’t judge. They’ll thank you.
The Future of OTC Medications
The FDA is overhauling the OTC system. By 2025, manufacturers will need to prove safety and effectiveness for every product. That means some old favorites could disappear. Around 15-20% of current OTC drugs may be pulled for lacking evidence.
Meanwhile, digital tools are rising. 63% of consumers now use apps to compare OTC products. AI-powered chatbots are starting to give personalized recommendations. And in 27 states, pharmacists can now prescribe certain OTC meds like emergency contraception without a doctor’s note.
But the biggest challenge? Consumer habits. We still buy multi-symptom formulas because they’re cheaper. But 61% of people say they’d prefer single-ingredient options. The market hasn’t caught up.
And then there’s the waste. $3.1 billion worth of unused OTC meds are thrown away every year. Expired. Opened. Forgotten. That’s not just money lost-it’s a public health risk. People dig through old cabinets and take things they shouldn’t.
Final Rule: Treat OTC Like Prescription
OTC doesn’t mean ‘no risk.’ It means ‘no doctor needed-for now.’ But you still need to be smart.
Here’s your checklist before you buy:
- Do I know the active ingredient?
- Am I already taking something with the same ingredient?
- Does my health condition make this risky?
- Is this for short-term use only?
- Have I checked the expiration date?
- Did I read the full label?
If you answer ‘no’ to any of these, stop. Talk to a pharmacist. Or wait. Or see a doctor.
Self-care is powerful. But only when it’s informed. The right OTC medication can make your day. The wrong one? It could change your life.
Can I take two different OTC pain relievers together?
No, unless a pharmacist or doctor tells you to. Mixing acetaminophen and ibuprofen is sometimes okay for short-term use, but only if you stick to the max dose of each and don’t exceed 24 hours. Most people mix them accidentally-like taking a cold medicine with acetaminophen and then adding ibuprofen. That’s how overdoses happen. Stick to one unless you’ve confirmed it’s safe.
Are store-brand OTC medications as good as name brands?
Yes. Store brands contain the same active ingredients, in the same doses, as name brands. The only differences are inactive ingredients (like dyes or flavors) and price. You’re paying for branding, not better medicine. If you’re trying to save money, store brands are a safe, effective choice.
What should I do if I take too much OTC medicine?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or your local emergency number. Don’t wait for symptoms. Acetaminophen overdose can damage your liver before you feel sick. Ibuprofen overdose can cause kidney failure or stomach bleeding. Time matters. Have the medicine bottle ready when you call-they’ll need the active ingredient and amount taken.
Can I give OTC medicine to my child?
Only if it’s labeled for children and you use the correct dose based on weight, not age. Never use adult formulas for kids. Liquid doses must be measured with the dosing cup or syringe that comes with the product-never a kitchen spoon. If you’re unsure, ask a pharmacist. Many pharmacies offer free pediatric dosing checks.
Why do some OTC meds require a photo ID to buy?
Products containing pseudoephedrine (like Sudafed) are restricted because they can be used to make illegal methamphetamine. The Combat Methamphetamine Epidemic Act of 2005 requires pharmacies to keep these behind the counter and ask for ID. You can still buy them, but you’ll need to show your ID and sign a log. This doesn’t apply to phenylephrine, which is now the more common decongestant in OTC cold meds.
Is it safe to use expired OTC medications?
Most OTC meds lose potency after expiration, but they rarely become toxic. However, antibiotics, liquid suspensions, and eye drops should never be used past their date-they can grow bacteria. For pain relievers or antacids, using them a few months past expiration is usually fine, but they may not work as well. When in doubt, throw it out. Expired meds aren’t worth the risk.

Chris Park
December 6, 2025 AT 21:58The FDA's OTC review? A corporate smokescreen. They approved 100,000 products but banned nothing for 50 years-until the CARES Act came along, right after the Big Pharma lobbying surge. You think labels are there to protect you? They're there to cover their asses. I've seen the internal memos. The real danger isn't acetaminophen-it's the fact that the same people who write the labels also own the patents on the drugs. You're not reading a label-you're reading a corporate script.
Inna Borovik
December 7, 2025 AT 22:43Let’s be real: 22% reading labels? That’s generous. I’ve watched my grandmother take three different cold meds because ‘they all help.’ She didn’t know they all had acetaminophen. She ended up in the ER. The problem isn’t just ignorance-it’s systemic. Pharmacies don’t train staff to explain labels. They train them to upsell. And the FDA? They’re slow, underfunded, and politically neutered. This isn’t a user error-it’s a failure of infrastructure.
Jackie Petersen
December 8, 2025 AT 17:19America’s OTC system is a joke. We let anyone walk in and buy 200 pills of pseudoephedrine with a photo ID and a signature. Meanwhile, in Germany, you need a prescription for Tylenol. We treat medicine like candy. And then we wonder why people overdose. It’s not about literacy-it’s about culture. We’ve normalized self-medication like it’s a patriotic duty. Wake up.
Annie Gardiner
December 9, 2025 AT 03:15I used to think OTC meds were harmless… until I started reading the fine print. Turns out, the ‘inactive ingredients’? They’re full of weird stuff-corn starch, FD&C red #40, even gluten in some pills. I have a sensitivity, and no one told me. I thought ‘natural’ meant safe. It doesn’t. The label doesn’t care if you’re allergic to dyes or have celiac. It just says ‘other ingredients.’ That’s not transparency. That’s negligence dressed up as regulation.
Myles White
December 11, 2025 AT 02:30One thing I’ve learned after working in pharmacy for 18 years: people don’t read the label because they don’t trust it. They’ve been burned before-by misleading ads, by inconsistent dosing, by brands that change formulations without warning. So they go with what ‘feels right.’ And honestly? I get it. The Drug Facts label is a masterpiece of bureaucratic design. It’s dense, confusing, and doesn’t account for real-life situations. If you’re a single mom with three kids and a headache, you’re not going to sit there and compare active ingredients. You need simplicity, not a legal document. The system needs to be redesigned for humans, not lawyers.
Saketh Sai Rachapudi
December 12, 2025 AT 03:41India has better OTC rules than the US. We have strict limits on combination drugs, mandatory pictograms for illiterate users, and pharmacy staff are legally required to counsel. In the US, you can buy 300 tablets of ibuprofen like it’s gum. That’s not freedom-that’s negligence. Why does America think its citizens are too dumb for basic regulation? We don’t let people buy guns without background checks. Why are pills any different?
joanne humphreys
December 13, 2025 AT 04:44I’ve been reading the labels for years now. It’s not perfect, but it’s the only thing standing between me and a hospital visit. I keep a spreadsheet of everything I take-even vitamins. I check for overlaps. I write down expiration dates. It’s not hard. It just takes 30 seconds. If you’re not doing this, you’re gambling with your liver. And no, you’re not too busy. Your health isn’t optional.
Arjun Deva
December 14, 2025 AT 21:44They say 'read the label'... but who wrote it? The same people who profit from your overdose. Acetaminophen? They knew the threshold was dangerous since the 80s. They just didn’t change it. Why? Because they make more money when you go to the ER. And then they sell you the next pill. It’s not a mistake. It’s a business model. The FDA? They’re on payroll. Don’t trust the label. Trust your gut. And if you’re feeling weird after taking something? Stop. Don’t wait. Call Poison Control. Even if you’re 'just being paranoid.'
Mayur Panchamia
December 16, 2025 AT 04:47Let’s be honest-this whole post is just fearmongering dressed up as ‘public service.’ You think people are dumb? They’re not. They’re tired. They’re overworked. They’ve been lied to by doctors, pharma ads, and now this ‘expert’ telling them to read 12 lines of tiny print before taking a Tylenol. We’ve turned medicine into a religion of suspicion. Meanwhile, in Japan, you can buy codeine OTC. In Canada, you can buy hydrocodone without a script. But here? We’re so scared of liability that we’ve made self-care a minefield. Maybe the problem isn’t the pills-it’s the paranoia.
Kenny Pakade
December 16, 2025 AT 08:44OTC meds are safe. The real problem? People who think they’re doctors. You don’t need to read the label. You need to trust your body. If it hurts, take a pill. If it doesn’t help, stop. If you feel weird, go to the doctor. Simple. Not rocket science. This post reads like a corporate compliance manual written by a guy who’s never taken anything stronger than aspirin. Stop scaring people. They’re not children.
brenda olvera
December 17, 2025 AT 19:25I’m from Mexico and we don’t have all these rules. You walk into any pharmacy, ask for something for your headache, and they hand you a pill. No ID. No label reading. No fear. And guess what? People don’t die from it. Maybe we don’t need all this complexity. Maybe we just need trust. Trust in our bodies. Trust in pharmacists. Trust in each other. Not more labels. Less.
Clare Fox
December 19, 2025 AT 07:36It’s funny how we treat medicine like it’s magic. We think if we take enough of it, the pain will disappear forever. But pain is a signal. OTC meds are just silence buttons. They don’t fix anything. They just let us ignore the problem until it’s too late. Maybe the real solution isn’t better labels-it’s better listening. To our bodies. To our symptoms. To the quiet voice saying, ‘this isn’t normal.’