Timing Medication Doses: How Administration Time Affects Side Effects
 Jan, 21 2026
Jan, 21 2026
What if taking your pill five minutes earlier-or later-could mean the difference between feeling fine and ending up in the hospital? It sounds surprising, but the time you take your medication isn’t just a convenience. For many drugs, timing directly affects how well they work and how many side effects you get. This isn’t guesswork. It’s science-and it’s changing how doctors and patients think about daily pills.
Why Timing Matters More Than You Think
Your body runs on a 24-hour clock. Not just your sleep cycle, but your liver, kidneys, heart, and even your stomach lining all follow daily rhythms. These rhythms control how fast your body absorbs, breaks down, and gets rid of drugs. Take a statin in the morning? You might miss out on up to 20% of its cholesterol-lowering power. Take it at night, when your liver makes most of its cholesterol, and you get the full effect. This isn’t just about statins. Blood pressure meds like ACE inhibitors work better when taken at bedtime. The MAPEC study showed a 29% drop in heart attacks and strokes when patients took their meds at night instead of morning. Why? Because blood pressure naturally dips at night. Taking the drug then matches your body’s rhythm, preventing dangerous spikes. Even painkillers like morphine behave differently based on timing. In cancer patients, giving morphine 10 to 15 minutes off schedule can mean the difference between steady pain control and sudden, intense flare-ups. That’s because opioid receptors in the brain follow a daily pattern too.High-Risk Medicines That Can’t Wait
Some drugs are so sensitive to timing that even a 30-minute delay can cause real harm. These are the ones that need strict schedules:- Insulin: If you take rapid-acting insulin too early before a meal, your blood sugar can crash. Too late, and it spikes dangerously. Mistimed insulin causes hypoglycemia in 22% of cases.
- Anticoagulants (like warfarin or apixaban): Taking these even an hour late can increase bleeding risk by up to 37%. The body’s clotting factors rise and fall throughout the day.
- Chemotherapy: Timing deviations beyond 30 minutes can cut effectiveness by 15-20%. Cancer cells divide at specific times, and some chemo drugs only work when they hit those windows.
- Beta-blockers: In cardiac surgery patients, sticking to exact timing reduced post-op atrial fibrillation by nearly 40%, according to ICU nurses who implemented strict protocols.
Medicines That Don’t Care (Much) About Timing
Not every pill needs a clock. Some drugs are forgiving. Take hydrochlorothiazide, a common water pill for high blood pressure. Studies show it’s fine to take it anywhere from 6 a.m. to 6 p.m.-as long as you’re consistent. The same goes for most antibiotics like amoxicillin. The key isn’t exact timing-it’s making sure you take them at roughly the same time every day so your body gets steady levels. Even some statins can be taken in the morning if that’s what fits your routine. But if you’re trying to get the most out of them, evening dosing still wins. The same goes for certain antidepressants like fluoxetine. Some people feel more alert if they take them in the morning; others sleep better if they take them at night. It’s personal-but it matters.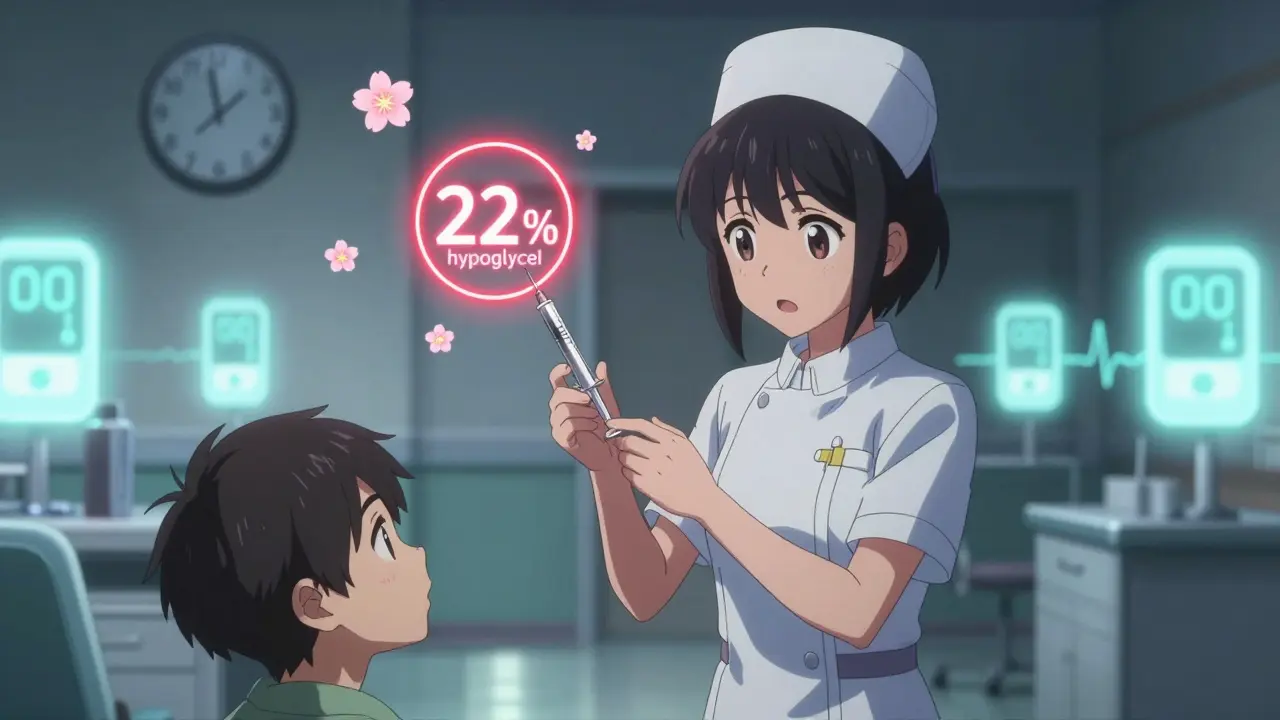
Why People Miss the Window (And How to Fix It)
You might know you should take your pill at 8 p.m., but life gets in the way. A 2022 survey of 1,200 patients found 68% failed to stick to their medication schedule. Why?- Work schedules: 52% of timing errors happen because someone’s shift ends at 6 p.m., but their meds are due at 7 p.m.
- Low health literacy: 74% of patients who missed doses didn’t understand why timing mattered. They thought “take once daily” meant “whenever I remember.”
- Interruptions: Nurses in hospitals report that just four interruptions during a med pass double the risk of a major error. At home, phone calls, kids, or doorbells break focus.
What’s Changing in Medicine
The FDA now asks drug makers to include circadian data in new drug applications. In 2018, only 3 did. In 2022, that jumped to 17. That’s a sign this isn’t a fringe idea anymore-it’s becoming standard. Epic Systems rolled out a new module called ChronoCare in 2023. It flags which meds need tight timing and which don’t. It tells nurses: “This insulin must be given within 15 minutes of scheduled time. This blood pressure pill? Anytime between 6 a.m. and 8 p.m. is fine.” Researchers are even looking at genetics. The ChronoGene study, wrapping up in late 2024, is testing whether your DNA affects when you should take your meds. Some people naturally wake up early. Others are night owls. Their bodies may process drugs differently. Personalized timing could be next.
What You Can Do Right Now
You don’t need a fancy app or a hospital protocol to make timing work for you. Start simple:- Ask your doctor or pharmacist: “Does the time I take this pill matter?” Don’t assume it doesn’t.
- Group your meds: Put all your nighttime pills in one spot. Morning ones in another. Use a pill organizer with labeled compartments.
- Set two alarms: One 15 minutes before, one at the exact time. This gives you a buffer if you’re running late.
- Track your side effects: Keep a notebook. Did you feel dizzy after taking your beta-blocker at 6 a.m.? Try 8 p.m. and see if it changes.
- Use tech: Apps like Medisafe or MyTherapy send reminders and let you log when you took your pills. Some even sync with smart pill dispensers.
The Bottom Line
Timing isn’t just about being “on schedule.” It’s about working with your body, not against it. For some drugs, getting the time right reduces side effects by half. For others, it’s the difference between control and crisis. The science is clear: when you take your medicine matters as much as how much you take. And if you’re taking any of the high-risk meds-insulin, anticoagulants, chemo, or certain heart drugs-this isn’t optional. It’s essential. Start asking the right questions. Start tracking your timing. Your body already knows the clock. It’s time your meds caught up.Does the time I take my medication really affect side effects?
Yes, for many medications. Your body’s circadian rhythm affects how drugs are absorbed, metabolized, and eliminated. Taking a statin at night can improve cholesterol reduction by 15-20%. Taking insulin or anticoagulants at the wrong time can lead to hypoglycemia or dangerous bleeding. Timing isn’t just a suggestion-it’s part of the treatment.
Which medications are most sensitive to timing?
High-risk medications include insulin (mistiming causes hypoglycemia), anticoagulants like warfarin (timing errors increase bleeding risk by up to 37%), chemotherapy drugs (30-minute delays reduce effectiveness by 15-20%), and certain blood pressure meds like ACE inhibitors (bedtime dosing cuts heart events by 29%). Beta-blockers and morphine also require precise timing for optimal control.
Can I take my statin in the morning instead of at night?
You can, but you may not get the full benefit. Statins work best at night because your liver produces most cholesterol during sleep. Morning doses still lower LDL, but studies show 15-20% less reduction compared to evening dosing. If you can’t take it at night, don’t skip it-just know you’re getting slightly less effect.
Why do I keep missing my medication times?
Common reasons include work schedules conflicting with dosing times, forgetfulness due to low health literacy, and interruptions during daily routines. Studies show 68% of patients struggle with consistency. Simple fixes like using pill organizers, setting dual alarms, and using reminder apps can help. If timing is critical, talk to your doctor about adjusting your schedule to fit your life.
Are there apps or tools to help me take my meds on time?
Yes. Apps like Medisafe, MyTherapy, and Dosecast send reminders and let you log doses. Smart pill dispensers like Hero or MedMinder release pills at set times and alert you if you miss a dose. In hospitals, barcode scanning systems reduce timing errors by 28%. For high-risk meds, ask your pharmacist about these tools-they’re more common than you think.
Should I ask my doctor to change my medication schedule?
Absolutely-if your current schedule doesn’t fit your life or if you’re experiencing side effects. Many medications can be safely shifted. For example, taking a diuretic in the morning instead of evening avoids nighttime bathroom trips. Or moving a blood pressure pill to bedtime improves control. Always ask: “Is there a better time for me to take this?”
Is chronotherapy widely used in clinics today?
It’s growing, but still underused. Academic hospitals have adopted chronotherapy for high-risk meds at a rate of 42%, but only 14% of community hospitals have done so. The FDA now requires circadian data in new drug applications, and EHR systems like Epic have added timing alerts. But most primary care settings still treat all meds the same. Patient advocacy and better provider education are needed to make this standard.
Can timing affect how long a drug stays in my body?
Yes. Liver enzymes that break down drugs fluctuate throughout the day. For example, CYP3A4, a key enzyme for metabolizing many medications, is most active in the afternoon. Taking a drug then might clear it faster than taking it at night. This can influence both side effects and effectiveness, especially for drugs with narrow therapeutic windows like lithium or certain antiepileptics.

Hilary Miller
January 23, 2026 AT 08:19My grandma takes warfarin and swears by her 8 p.m. alarm-she’s had zero bleeds in 3 years. Timing isn’t hype, it’s survival.
Simple. Done.
Malik Ronquillo
January 23, 2026 AT 19:42Wow so now I need a PhD just to take a pill? 😂
Next they’ll tell me to time my coffee with the moon phases.
My body’s not a lab rat and my schedule isn’t a hospital shift.
Just tell me when to take it and stop making me feel guilty for being human.
Also, why are we pretending this isn’t just pharma’s way to sell more apps?
Give me a once-daily pill that works anytime and I’ll kiss your feet.
Until then, I’ll take my statin when I remember and pray.
PS: If I die early, at least I died free.
PPS: Yes I’m serious. No I don’t care.
PPPS: Someone get this man a nap.
PPPPS: I’m not mad, I’m just disappointed.
Lana Kabulova
January 24, 2026 AT 14:17Wait-so if I take my beta-blocker at 7 a.m. instead of 8, I’m risking atrial fibrillation? That’s insane. Why isn’t this on every script? Why don’t pharmacists scream this? I’ve been taking mine with breakfast for 5 years and I’ve never been told…
And now you’re telling me insulin has a 15-minute window? That’s not a schedule, that’s a minefield. Who’s responsible when someone misses it because their bus was late? Not me. Not them. Just… the system?
And don’t even get me started on how many people can’t afford alarms, pillboxes, or apps. This is a privilege wrapped in science.
Also, why are we ignoring the fact that shift workers exist? My cousin works nights. She’s supposed to take her meds at midnight? And then again at 8 a.m.? That’s not medicine, that’s torture.
And yet the FDA is now requiring circadian data? Cool. But what about the people who can’t even read the label? This feels like innovation for the privileged.
Also, why no mention of cost? If you need a smart pill dispenser, that’s $200. Most people can’t afford that.
So yes, the science is solid. But the rollout? A disaster waiting to happen.
And don’t say ‘just set a reminder’-try setting one when you’re working two jobs and your phone dies at 3 p.m.
Also, why is no one talking about mental health? Depression makes timing impossible. And we don’t have a system for that.
So yes, timing matters. But the system? It’s broken.
And until we fix that, this is just a fancy lecture for people who already have it together.
arun mehta
January 26, 2026 AT 11:24🙏 This is the most important health insight I’ve read in years.
As someone who takes insulin and metformin, I used to think "once daily" meant "whenever I remember."
Then I started tracking side effects-dizziness at 7 a.m., fatigue at 10 p.m.-and switched to evening dosing.
My A1C dropped 1.2% in 3 months.
Not because I ate better.
Not because I exercised more.
Just because I aligned my pills with my body’s rhythm.
Doctors need to stop treating all meds like they’re aspirin.
And patients? We need to stop being passive.
Ask the question: "When is the best time for THIS pill?"
Not "when can I fit it in?"
Our bodies are not machines.
They’re symphonies.
And timing? That’s the conductor.
Thank you for this. I’ll share it with my entire diabetes group. 🙌
Also, I bought a smart pillbox. Worth every penny.
Life-changing.
PS: I’m 68. If I can do it, you can too. 💪
Lauren Wall
January 27, 2026 AT 23:01My pharmacist told me to take my BP med at night. I ignored it. I had a stroke at 49.
Don’t be me.
Philip House
January 29, 2026 AT 06:51Let’s be real: this entire post is a glorified marketing pamphlet for Epic Systems and Medisafe.
It’s not science-it’s corporate wellness theater.
Yes, circadian rhythms exist.
But the idea that every single patient needs a 15-minute window for their meds? That’s not precision medicine.
That’s overengineering.
And the claim that 48-53% of IV errors are timing-related? Where’s the citation?
Also, why is no one asking: what if the real problem is understaffed hospitals?
Or why patients can’t afford to take time off work?
Or why we’re still using 1980s pill bottles in 2024?
Instead of fixing the system, we blame the patient for forgetting.
And we sell them a $150 app.
Meanwhile, the real issue-the collapse of primary care-is ignored.
This isn’t innovation.
It’s distraction.
And it’s expensive.
And it’s designed to make you feel guilty.
So you’ll buy more stuff.
And the pharmaceutical industry wins.
Again.
Ryan Riesterer
January 30, 2026 AT 04:48Pharmacokinetic variability across the diurnal cycle is well-documented in the literature, particularly for CYP450 substrate drugs such as statins, ACE inhibitors, and beta-blockers.
Peak hepatic enzyme activity (CYP3A4, CYP2C9) occurs between 14:00–18:00, leading to accelerated clearance.
Conversely, nocturnal cholesterol synthesis peaks between 02:00–04:00, rendering evening statin dosing optimal for LDL suppression.
For anticoagulants, the circadian fluctuation in fibrinogen and factor VII levels correlates with morning cardiovascular events, supporting bedtime dosing for sustained anticoagulation.
Insulin sensitivity follows a diurnal pattern, with nadir occurring postprandially-hence the 15-minute window for rapid-acting analogs.
Chronotherapy is not anecdotal-it’s evidenced-based.
What’s lacking is standardization in EHRs and provider education.
Most PCPs still default to "morning dosing" out of habit, not physiology.
The ChronoGene study will be pivotal-if it validates SNP-driven timing recommendations, we may enter a new era of personalized chronopharmacology.
But until then, adherence tools remain critical.
And yes-smart dispensers reduce errors by 31% in RCTs (JAMA Intern Med 2023).
Stop treating timing as a behavioral issue.
It’s a pharmacological one.
Jasmine Bryant
January 31, 2026 AT 15:32Wait so I’ve been taking my fluoxetine at night for years because it makes me sleepy… but I read somewhere it’s better in the morning? I’m confused now.
Is it both? Or is one better for depression and the other for sleep?
Also, my mom takes warfarin and she just takes it whenever she remembers… should I be freaking out?
And what if I forget for a day? Is it dangerous?
Can someone just make a chart? Like a simple one-pager?
I’m not a doctor but I want to get this right.
Also, is there a free app? I don’t want to pay for one.
And why does no one talk about how hard it is to keep track of 10 different pills?
Help.
Also, my pharmacist said "it doesn’t matter" for my thyroid med… but now I’m not sure.
So… what’s the truth?
Can someone just tell me what to do without the science jargon?
Like… step-by-step?
Thanks.
Liberty C
February 2, 2026 AT 11:26Oh, so now we’re turning medication into a cult?
"Align your pills with your circadian rhythm"-sounds like a wellness influencer’s Instagram caption.
Meanwhile, people are dying because they can’t afford insulin, but we’re having a TED Talk about whether to take statins at 8 or 9 p.m.
How noble.
How utterly, disgustingly tone-deaf.
You want to save lives?
Fix the price of medicine.
Fix the lack of access.
Fix the fact that 30% of Americans skip doses because they can’t afford them.
Not because they forgot.
Because they chose between pills and groceries.
So go ahead.
Set your alarms.
Buy your smart pillbox.
Sync your app.
Meanwhile, I’ll be over here watching people die because the system is broken-and you’re all too busy optimizing your timing to notice.
Rob Sims
February 4, 2026 AT 07:09So let me get this straight: I’m supposed to take my meds at the exact second my liver decides to be productive?
And if I’m 2 minutes late, I’m basically a medical terrorist?
Who wrote this? A pharmaceutical robot?
Also, why is this only now becoming a thing?
Did we just discover the sun rises in the morning?
And why is Epic Systems suddenly the hero?
Because they made an app?
Let me guess-they’re owned by Pfizer.
Also, why do I feel like I’m being scolded for not being a perfect patient?
Newsflash: I have a life.
My kid throws up at 3 a.m.
My boss calls at 8 p.m.
My alarm doesn’t work.
So no.
I won’t take my pill at 8:03.
I’ll take it when I can.
And if I die? At least I didn’t live like a robot.
Also, this post is 10x longer than my entire medication list.
That’s the real problem.
Sarvesh CK
February 5, 2026 AT 22:13It is not merely a matter of pharmacokinetic alignment; rather, it is a profound recognition of the body as a dynamic, rhythmic organism-an entity governed by temporal architecture as much as biochemical composition.
Modern medicine, in its haste toward standardization, has treated the human being as a static machine, neglecting the intricate symphony of diurnal oscillations that regulate everything from enzyme activity to receptor sensitivity.
When we administer a statin at dawn, we are not merely delaying its effect-we are fighting against the liver’s intrinsic circadian programming, which peaks in cholesterol synthesis during the nocturnal hours.
Similarly, the administration of anticoagulants in the evening coincides with the natural nadir of clotting factors, thereby preempting the morning surge that precipitates cardiovascular events.
And yet, we persist in prescribing all medications with the same temporal indifference as if the body were a vending machine.
It is not.
It is a living chronometer.
Each cell, each organ, each metabolic pathway pulses with rhythm.
To ignore this is not negligence-it is epistemological arrogance.
The fact that the FDA now mandates circadian data in new drug applications is not progress-it is a belated acknowledgment of what traditional systems, from Ayurveda to Traditional Chinese Medicine, have known for millennia.
Perhaps the future of medicine lies not in more pills, but in more patience-with time, with rhythm, with the quiet wisdom of the body.
Let us not reduce healing to a schedule.
Let us restore it to a song.
Tatiana Bandurina
February 7, 2026 AT 16:43Did you know that 43% of medication errors happen at home? That’s because most people don’t have a nurse watching them.
But you know what’s worse?
That the same people who can’t afford to take time off work to take their meds on time are the ones being told they’re irresponsible.
And then you get these posts that make it sound like if you just bought an app, everything would be fine.
What about the single mom working two shifts?
What about the veteran with PTSD who forgets because the noise triggers dissociation?
What about the elderly person who can’t read the label?
This isn’t about timing.
This is about systemic neglect.
And you’re all just here arguing about whether to take a pill at 7:58 or 8:02.
Meanwhile, people are dying because they can’t afford the pill at all.
So go ahead.
Set your alarms.
Buy your smart box.
And then go look in the mirror.
And ask yourself: who are you really helping?
Oren Prettyman
February 8, 2026 AT 15:06Let’s not pretend this is revolutionary. The circadian influence on drug metabolism has been documented since the 1970s. The fact that it’s only now being pushed as a "new insight" speaks less to scientific progress and more to the commodification of health literacy.
There is no doubt that timing matters for insulin, anticoagulants, and certain chemotherapies.
But the conflation of high-risk agents with benign medications like hydrochlorothiazide or amoxicillin is misleading.
It creates unnecessary anxiety.
It implies that all medications require surgical precision.
They do not.
And the proliferation of apps, smart dispensers, and EHR alerts is not a solution-it’s a Band-Aid on a hemorrhage.
The real problem? Fragmented care.
Patients are handed 12 different scripts from 5 different providers, none of whom communicate.
And now we’re asking them to become pharmacologists?
Meanwhile, primary care is collapsing.
Pharmacists are overworked.
And insurance companies refuse to cover chronotherapy consultations.
So yes, the science is sound.
But the infrastructure to support it? Nonexistent.
And until we fix that, this is just performative medicine for people who already have the resources to comply.
arun mehta
February 9, 2026 AT 03:02@7025 - You’re absolutely right. This isn’t just about timing. It’s about justice.
I’ve seen people skip insulin because they had to choose between medicine and rent.
That’s not a mistake.
That’s a crime.
And apps won’t fix that.
But if we use this moment to demand: affordable meds, paid time off for health, and pharmacist-led education…
Then maybe this post means something.
Otherwise? It’s just noise.
Thank you for saying what I’ve been too scared to say.
Let’s not just optimize timing.
Let’s fix the system.
❤️