Obesity Pathophysiology: How Appetite and Metabolism Go Wrong
 Dec, 30 2025
Dec, 30 2025
Most people think obesity is just about eating too much and moving too little. But that’s not the full story. Under the surface, your body’s hunger signals, metabolism, and brain wiring are all stuck in a broken loop. This isn’t laziness. It’s biology. And it’s why losing weight feels impossible for so many, even when they’re doing everything "right."
The Brain’s Hunger Switches Are Out of Order
Your hypothalamus, a tiny region deep in your brain, acts like the control center for hunger and fullness. It doesn’t guess - it listens. It picks up signals from fat cells, your gut, and your pancreas, then tells you when to eat and when to stop. Two groups of neurons in this area are the main players: POMC neurons that say "stop eating," and NPY/AgRP neurons that scream "eat more." In a healthy body, these two teams balance each other. But in obesity, that balance collapses. Leptin, the hormone your fat cells release to tell your brain you have enough stored energy, stops working. You have high leptin levels - sometimes 30 to 60 ng/mL - but your brain ignores it. This is called leptin resistance. It’s like your car’s fuel gauge is stuck on empty, even though the tank is full. So your brain keeps telling you to eat, even when you’re carrying extra weight.At the same time, ghrelin - the hunger hormone - stays too high. Normally, ghrelin spikes before meals, then drops after you eat. In obesity, it doesn’t fall back down like it should. You feel hungrier, more often. And when you do eat, your brain doesn’t get the full signal as quickly. That’s why you might finish a big meal and still feel unsatisfied.
Insulin and the Metabolic Trap
Insulin isn’t just for blood sugar. It also talks to your brain to reduce appetite. In lean people, insulin levels rise after eating - from about 5-15 μU/mL fasting to 50-100 μU/mL after a meal - and help shut down hunger. But in obesity, insulin resistance kicks in. Your body needs more and more insulin to do the same job. And that high insulin doesn’t just mess with your blood sugar - it also blunts the signal to your brain that you’re full.Here’s the cruel twist: high insulin promotes fat storage. So even if you eat less, your body holds onto calories as fat instead of burning them. This creates a cycle: more fat → more insulin → more fat storage → more hunger → more eating. It’s not about willpower. It’s about your body’s chemistry working against you.
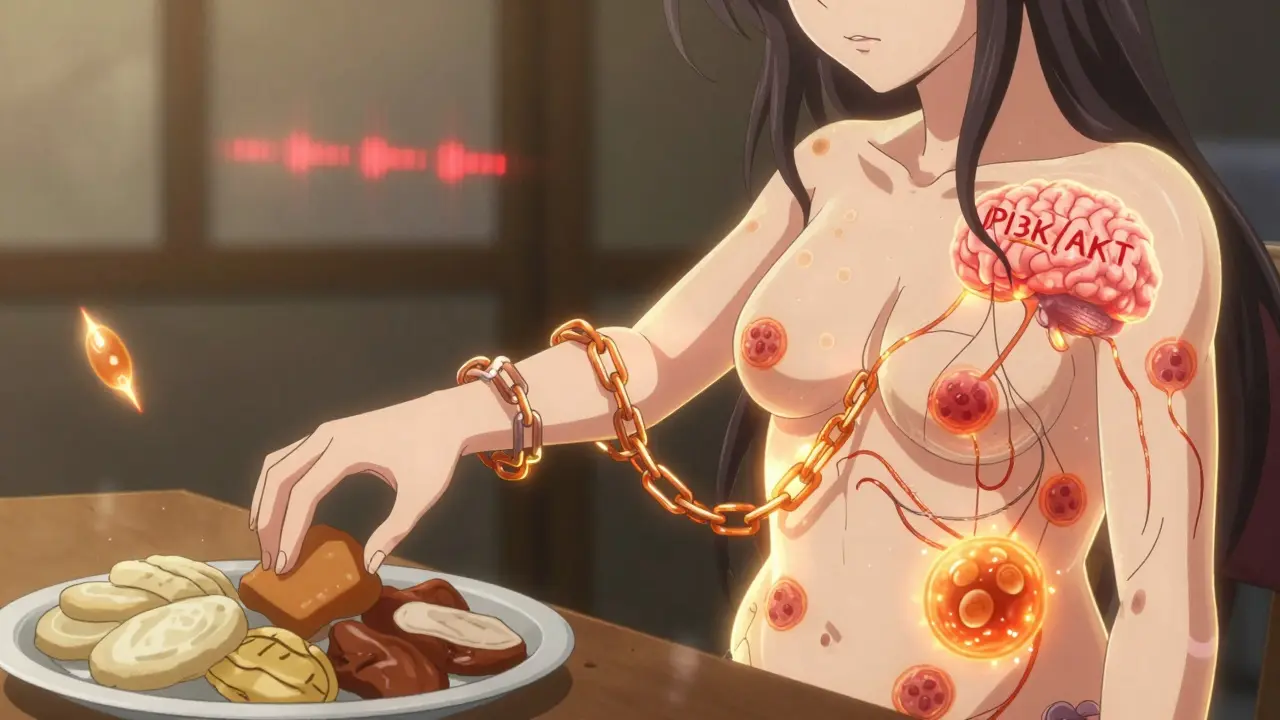
The Broken Pathways Inside Your Cells
It’s not just hormones - it’s what happens inside brain cells after those hormones arrive. Leptin and insulin both rely on the PI3K/AKT pathway to send their "stop eating" message. But in obesity, this pathway gets blocked. Inflammation, excess fat, and high sugar intake trigger molecules like JNK that interfere with the signal. Think of it like a broken phone line - the call is being made, but the message never gets through.Even the mTOR system, which normally helps regulate energy balance, gets tangled up. When it’s overactive, it can make your brain less sensitive to fullness cues. And when you combine this with a diet full of ultra-processed foods - high in sugar, fat, and salt - your brain’s reward system goes into overdrive. The same brain circuits that once helped you seek out calorie-dense foods for survival now drive you to overeat, even when you’re not hungry.
Why Some People Are More Susceptible
Not everyone who eats the same way gains the same amount of weight. Genetics play a big role. Rare mutations in genes like POMC or LEPR can cause severe obesity from childhood - but these affect fewer than 50 people worldwide. For most, it’s not one broken gene. It’s many small changes that add up.Women after menopause are a clear example. Estrogen helps regulate appetite and energy use. When estrogen drops, women gain more belly fat and eat more. Studies show estrogen receptor knockout mice eat 25% more and burn 30% less energy. In humans, it’s common to gain 12-15% more central fat within five years of menopause - even with no change in diet or activity.
Another group with clear biological drivers: people with Prader-Willi syndrome. They have abnormally low levels of pancreatic polypeptide (PP), a hormone that slows digestion and reduces hunger. Their PP levels are often 15-25 pg/mL, while normal is 50-100 pg/mL. That’s why they feel constant hunger, no matter how much they eat.
What Treatments Actually Work - and Why
Most diets fail because they don’t fix the biology. But new drugs are finally targeting the root causes. Semaglutide, originally for diabetes, mimics GLP-1 - a gut hormone that slows stomach emptying and tells your brain you’re full. In trials, people lost an average of 15% of their body weight. Setmelanotide works directly on the melanocortin-4 receptor (MC4R), bypassing leptin resistance. In people with rare genetic forms of obesity, it cuts weight by 15-25%.These drugs don’t just reduce appetite. They reset the brain’s set point. That’s why weight loss is sustained - not just while taking the drug, but for months after. The brain finally starts believing you’re not starving anymore.
And now, researchers have found a new group of neurons right next to the hunger and fullness cells in the hypothalamus. When activated, they shut down eating within two minutes. This could lead to even more precise treatments - ones that turn off hunger without side effects.
The Bigger Picture: It’s a Disease, Not a Choice
Obesity affects 42.4% of U.S. adults and nearly tripled globally since 1975. It’s linked to 2.8 million deaths a year and costs the U.S. healthcare system $173 billion annually. Yet, it’s still wrongly seen as a failure of discipline.The science is clear: obesity is a chronic disease of metabolic and neurological dysfunction. Your appetite isn’t broken because you’re weak. It’s broken because your body’s signaling system has been hijacked by excess fat, inflammation, and poor diet. The good news? We now have tools to fix it - not by willpower, but by biology.
The next frontier isn’t just weight loss. It’s restoring balance. Treatments that combine appetite control with improved metabolism - like those now in phase 2 and 3 trials - could change everything. For the first time, we’re not just treating symptoms. We’re fixing the system.

Harriet Hollingsworth
December 30, 2025 AT 15:14This is why people need to stop making excuses. If you’re overweight, you’re just lazy. No amount of science changes that. I’ve seen people lose weight with willpower alone. Stop blaming your brain.
It’s not a disease. It’s a choice. And choices have consequences.
linda permata sari
December 31, 2025 AT 09:13OMG I CRIED reading this. 😭
My mom had Prader-Willi. She ate until she passed out. People called her greedy. They didn’t know her brain was screaming for food. This isn’t about snacks. It’s about survival mode on repeat.
Thank you for saying it out loud. We’re not broken. We’re biologically hijacked.
Brandon Boyd
January 2, 2026 AT 06:47YES. This is the message we NEED to hear. You’re not failing - your biology is stuck. And guess what? It can be rewired.
I lost 80 lbs with semaglutide. Not because I was ‘stronger’ - because the constant hunger finally turned off. I could breathe again.
If you’re struggling, please don’t give up. The science is here. The tools are real. You’re not alone. Keep going - your body is fighting for you, even when it feels like it’s not.
One step. One day. One meal at a time. You got this 💪
John Chapman
January 3, 2026 AT 15:45THIS. IS. LIFE-CHANGING. 🤯🔥
I used to think obesity was just ‘bad habits.’ Now I get it - my insulin was screaming like a broken alarm clock and my brain was deaf to it. Semaglutide didn’t just help me lose weight - it gave me my mind back.
Stop shaming people. Start funding research. This isn’t a moral issue - it’s a medical emergency. We need this stuff covered by insurance NOW. 🙏❤️
Urvi Patel
January 4, 2026 AT 12:44Joy Nickles
January 5, 2026 AT 06:31Emma Hooper
January 5, 2026 AT 09:27Oh honey. You’re not lazy. You’re not weak. You’re not broken. You’re a biological masterpiece that got glitched by sugar, stress, and silence.
That hypothalamus? It’s been screaming into a void for years. And now? We’re finally giving it a microphone.
Every time someone says ‘just eat less,’ they’re kicking a drowning person while they’re underwater. Don’t be that person. Be the one who says: ‘I see you. I believe you. Let’s fix this.’
Martin Viau
January 6, 2026 AT 13:18Typical American medical-industrial complex propaganda. In Canada, we don’t need $10,000 drugs to lose weight. We just... don’t eat junk. Simple. Our healthcare system doesn’t fund this nonsense. It’s all about profit, not physiology. This article is a marketing pamphlet dressed in jargon.
Also, leptin resistance? That’s not even proven in humans. Just mouse studies. Don’t fall for the hype.
Marilyn Ferrera
January 6, 2026 AT 20:59Thank you. This is the clearest, most compassionate summary of obesity biology I’ve ever read.
It’s not about discipline. It’s about signaling. And we’ve been treating a neurological disorder like a moral failing.
Finally, the science is catching up to the lived experience of millions.
Let’s stop the stigma. Start the treatment.
Robb Rice
January 8, 2026 AT 07:32I appreciate the depth of this post. As someone who’s struggled with weight for decades, I’ve been told I’m lazy, weak, undisciplined - all while my body was screaming for help.
Thank you for explaining the science without judgment. I’ve started semaglutide last month. The difference? I no longer feel like I’m in a war with my own brain.
It’s not a cure. But it’s the first tool that actually works with my biology, not against it.
For the first time in 20 years… I feel hope.