Managing Diarrhea with Celiac Disease: Practical Gluten Sensitivity Tips
 Oct, 10 2025
Oct, 10 2025
Celiac Disease Diarrhea Management Checklist
Use this checklist to track your progress in managing celiac disease-related diarrhea. Select all applicable items below to get personalized recommendations.
Your Personalized Management Plan
Quick Takeaways
- Identify hidden gluten sources and avoid cross‑contamination.
- Stay hydrated with electrolyte‑rich fluids to replace losses from diarrhea.
- Consider low‑FODMAP foods and targeted probiotics to calm the gut.
- Track symptoms with a diary and work with your doctor on follow‑up testing.
- Know when to investigate other culprits like lactose intolerance or IBS.
Dealing with celiac disease diarrhea can feel overwhelming, but the right steps can bring relief.
Understanding the Link Between Diarrhea and Celiac Disease
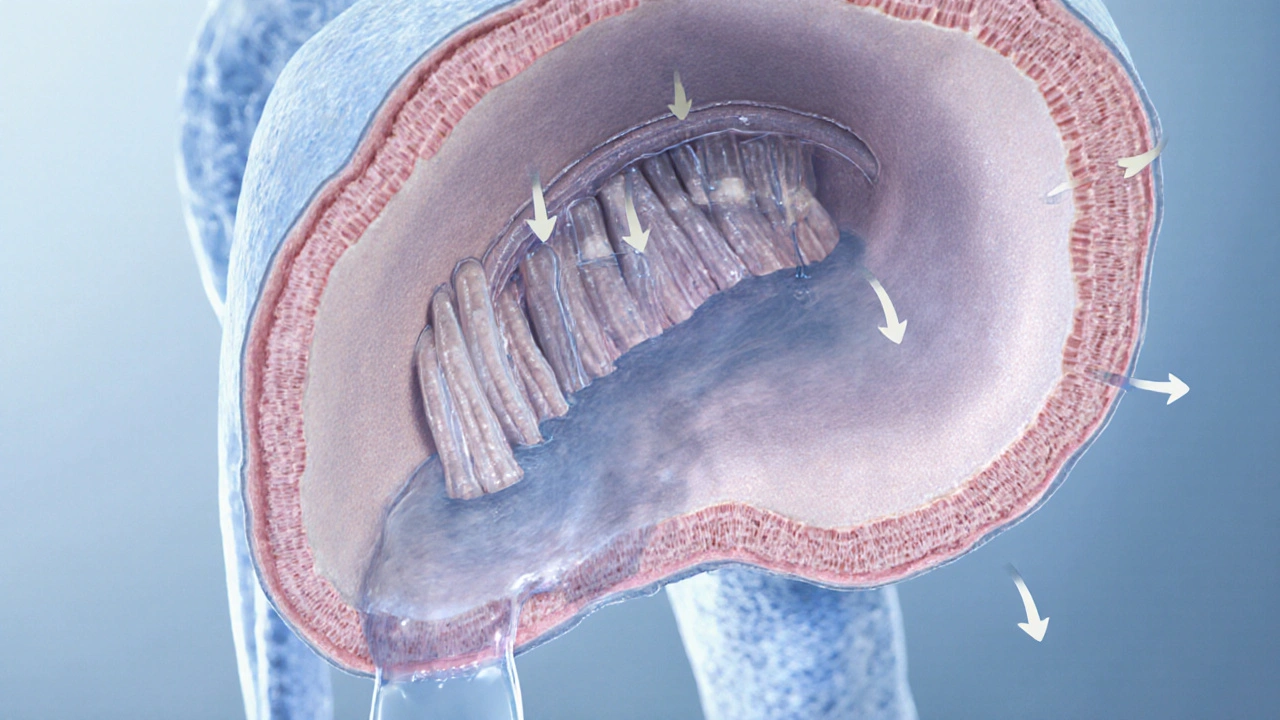
When building a healthier gut, Celiac Disease is an autoimmune disorder where the immune system reacts to gluten, damaging the small intestine’s lining. The damage reduces the intestine’s ability to absorb nutrients and water, often resulting in watery, frequent stools.
Gluten is a protein found in wheat, barley, and rye that triggers the immune response in people with celiac disease. Even tiny amounts can set off inflammation, leading to the classic "gliadin‑induced" diarrhea.
Because the villi (tiny finger‑like projections) become flattened, the gut can’t re‑absorb fluid efficiently, pushing excess water into the colon and causing diarrhea.
Core Strategies for Managing Gluten Sensitivity
Adopting a strict Gluten‑Free Diet is the only proven treatment for celiac disease, requiring elimination of all gluten‑containing ingredients. Here’s how to make it work:
- Read labels obsessively. Look for the gluten‑free symbol and scan the ingredient list for hidden sources like malt flavoring, modified food starch, or hydrolyzed vegetable protein.
- Watch out for cross‑contamination. Cross‑Contamination is the accidental transfer of gluten from contaminated surfaces, utensils, or shared cooking equipment. Use separate toasters, cutting boards, and cookware, and always rinse dishes before reuse.
- Choose whole‑food staples. Brown rice, quinoa, millet, buckwheat, and certified gluten‑free oats form a nutritious base without hidden gluten.
- Plan meals ahead. Batch‑cook soups, stews, and sauces in bulk, then freeze individual portions to avoid last‑minute temptations.
Sticking to these basics dramatically reduces the trigger that fuels diarrhea.

Hydration and Electrolyte Balance
Frequent watery stools deplete sodium, potassium, magnesium, and bicarbonate. Replenishing these electrolytes prevents cramps, dizziness, and fatigue.
- Oral rehydration solutions. Commercial mixes (e.g., Pedialyte) or homemade recipes-1 liter water, 6 teaspoons sugar, ½ teaspoon salt-restore balance quickly.
- Broths and soups. Low‑sodium bone broth provides fluids plus collagen, which may aid gut healing.
- Electrolyte‑rich foods. Bananas, avocados, boiled potatoes (with skin), and coconut water are gentle on the gut.
Aim for 1.5-2L of fluid a day, more if diarrhea is severe.
Supporting Your Gut: Probiotics, Fiber, and Low‑FODMAP Choices
While a gluten‑free diet removes the primary insult, the gut microbiome often needs extra help to regain stability.
- Targeted probiotics. Strains such as Lactobacillus rhamnosus GG and Bifidobacterium lactis have shown promise in reducing stool frequency for celiac patients. Choose a product with at least 10billion CFU per dose.
- Gentle soluble fiber. Foods like peeled apples, carrots, and chia seeds add bulk without aggravating excess gas.
- Low‑FODMAP diet. Low‑FODMAP Diet is a short‑term dietary approach that limits fermentable carbohydrates to reduce bloating and diarrhea. After a 2‑week trial, re‑introduce foods gradually to identify specific triggers.
Combining these strategies often smooths out the transition period after going gluten‑free.
When Diarrhea Persists: Check for Additional Triggers
If stools remain loose after several weeks on a strict gluten‑free plan, consider these common co‑factors:
- Lactose Intolerance. Damage to the villi can temporarily reduce lactase enzyme levels. Try a 2‑week lactose‑free trial; improvement suggests secondary lactose intolerance.
- Irritable Bowel Syndrome (IBS). Overlap symptoms can mask underlying celiac disease. A low‑FODMAP trial helps differentiate.
- Infections or parasites. Stool tests for Clostridioides difficile or giardia are warranted if diarrhea is acute, bloody, or accompanied by fever.
- Medications. Certain antibiotics, NSAIDs, and even high‑dose iron supplements can irritate the gut.
Working with a gastroenterologist to run targeted labs (tTG‑IgA, EMA, stool PCR) will clarify the root cause.

Monitoring and Follow‑Up
Effective management is an ongoing process. Keep a symptom diary noting:
- Food items and portion sizes
- Timing of meals vs. bowel movements
- Hydration intake and any electrolyte supplements
- Medication changes or stress events
Share this log with your doctor during follow‑up appointments. Repeat serology (tTG‑IgA) at 6‑12months to confirm that gluten exposure has dropped to negligible levels. Endoscopic biopsies are rarely needed once serology normalizes, but they remain the gold standard if symptoms persist.
Quick Comparison: Gluten‑Free vs. Low‑FODMAP
| Aspect | Gluten‑Free Diet | Low‑FODMAP Diet |
|---|---|---|
| Primary Goal | Eliminate gluten to stop immune attack | Reduce fermentable carbs to ease gas and diarrhea |
| Duration | Lifetime for celiac patients | 2-6 weeks short‑term, then re‑introductions |
| Typical Foods Included | Rice, quinoa, certified gluten‑free oats | Low‑FODMAP fruits (banana, berries), limited grains (gluten‑free oats, rice) |
| Risk of Nutrient Gaps | Fiber & iron can be low; needs supplementation | Calcium & vitamin D may drop; monitor intake |
| Complexity | Label reading is essential; cross‑contamination watch | Portion tracking & phased re‑introduction required |
Frequently Asked Questions
Can I have occasional gluten without worsening diarrhea?
For most people with celiac disease, even a tiny amount of gluten can trigger an immune response and cause diarrhea. Accidental exposure is common, but intentional “gluten holidays” are not recommended because they can reset the immune system and prolong healing.
How long does it take for diarrhea to improve after going gluten‑free?
Most patients notice a reduction in stool frequency within 2-4 weeks, but full recovery of the intestinal lining can take 6-12 months. Staying hydrated and adding probiotics can speed up the early relief phase.
Should I avoid all dairy while managing celiac‑related diarrhea?
Not necessarily. However, secondary lactose intolerance is common after intestinal damage. Try a short lactose‑free trial; if symptoms improve, limit dairy or use lactase enzyme supplements.
Are over‑the‑counter anti‑diarrheal meds safe for celiac patients?
Loperamide can be used for occasional flare‑ups, but it doesn’t address the underlying gluten trigger. If diarrhea is severe or persistent, focus on diet and hydration first, and consult a doctor before regular use.
What lab tests confirm that my gut is healing?
Serum tissue transglutaminase IgA (tTG‑IgA) levels should drop to normal within 6-12 months of strict gluten avoidance. In some cases, a follow‑up endoscopy with duodenal biopsy provides visual confirmation of villous recovery.

Sara Spitzer
October 10, 2025 AT 16:29While the checklist is a solid start, the article could benefit from clarifying the distinction between primary gluten avoidance and secondary lactose intolerance. The term “gliadin‑induced” is a bit redundant; gliadin is a component of gluten, so simply saying “gluten‑induced” would suffice. Also, the hydration section should cite the recommended oral rehydration solution ratio more precisely. A brief note on the possible need for iron supplementation in celiac patients would round out the nutrient‑gap discussion. Overall, the structure is logical, but a tighter edit would improve readability.
Hayden Kuhtze
October 14, 2025 AT 06:12Because gluten is the villain, any cameo is a crime scene.
Craig Hoffman
October 17, 2025 AT 19:55Probiotics can help, but pick the strains that have research behind them. Lactobacillus rhamnosus GG and Bifidobacterium lactis are good choices. Stick to at least 10 billion CFU per dose. Also, remember that a gluten‑free diet alone won’t fix a leaky gut overnight.
Terry Duke
October 21, 2025 AT 09:38Great job on putting together such a thorough guide! 🎉 It's impressive how many practical tips are covered, from label reading to electrolyte balance. Remember that staying motivated during the transition is key, and celebrating small victories-like a week without accidental gluten-can boost morale! If you ever feel overwhelmed, taking a short break to relax can actually help your gut heal faster. Keep sharing these resources; they really make a difference for the community! 🙌
Chester Bennett
October 24, 2025 AT 23:21One thing to keep in mind is that nutrient deficiencies often sneak in with a strict gluten‑free regimen. Iron, calcium, and certain B‑vitamins can be low, so a periodic blood test is wise. Pairing the diet with a well‑chosen multivitamin can fill those gaps without overcomplicating meals. Also, involving a dietitian early on ensures you’re getting a balanced intake. The checklist could include a reminder to schedule that professional appointment.
Emma French
October 28, 2025 AT 12:03It’s essential to monitor symptoms daily; a simple diary can reveal patterns you might otherwise miss. Don’t underestimate the impact of stress-mental health plays a big role in gut function. If diarrhea persists beyond four weeks despite strict adherence, consult your gastroenterologist promptly.
Debra Cine
November 1, 2025 AT 01:46Loved the clear tables! 😊 They make the comparison between gluten‑free and low‑FODMAP super easy to grasp. Keep those visual aids coming-they’re a lifesaver for newcomers.
Rajinder Singh
November 4, 2025 AT 15:29Behold, the silent battle within the duodenum, where each stray grain of wheat becomes a lance of torment. The author hath captured this strife with commendable vigor, yet the narrative could yet ascend to epic stature. By invoking the mythic triumph of healed villi, the piece would inspire readers to persevere. Let us not forget the humble broth, a potion of solace for the weary gut.
chuck thomas
November 8, 2025 AT 05:12The journey of healing mirrors the ancient quest for knowledge-both require patience, vigilance, and humility. As we chart our meals, we also chart the contours of our inner resilience. Let each symptom be a teacher, not an adversary, guiding us toward deeper self‑awareness.
Gareth Pugh
November 11, 2025 AT 18:55Think of gluten as the unwanted guest at a dinner party; politely show it the door. Then invite the vibrant, low‑FODMAP friends to the table.
Illiana Durbin
November 15, 2025 AT 08:38For those still experiencing occasional bloating, a short trial of soluble fiber can be beneficial. Start with small portions of peeled apples or carrots and observe the response. Gradual adjustments tend to yield the most sustainable results.
anshu vijaywergiya
November 18, 2025 AT 22:20Picture the gut as a bustling city, its streets clogged by rogue gluten traffickers. When the gates finally close, the citizens-your villi-begin to rebuild, brick by brick. Yet the shadows of lactose intolerance linger, whispering doubts in quiet corners. With courage and the right probiotic allies, you can restore harmony to this metropolis. Embrace the journey; the sunrise after the storm is worth every step.
Jackson Whicker
November 22, 2025 AT 12:03It is a lamentable truth that many proclaim mastery over their diet, yet remain shackled by ignorance-a modern tragedy befitting the most somber of Greek dramas. The author, in a commendable attempt, furnishes a checklist, but the very act of reducing complex pathology to bullet points borders on hubris. One must recognize that celiac disease is not merely a culinary inconvenience; it is an autoimmune siege that ravages the intestinal citadel. To suggest that a mere “low‑FODMAP trial” can substitute for rigorous serological monitoring is, frankly, a disservice. Moreover, the oversight of vitamin D and calcium deficiencies betrays a superficial grasp of the condition’s systemic reach. While the inclusion of probiotic strains is a step forward, the lack of dosage specificity undermines its utility. The narrative also neglects to address the psychosocial burden-social isolation at gatherings, the perpetual fear of cross‑contamination, the erosion of trust in food labeling. Such omissions reveal a gap between academic discourse and lived experience. The article could have been fortified by citing recent meta‑analyses that elucidate the modest benefits of certain prebiotics in celiac remission. Additionally, a nuanced discussion of secondary lactose intolerance, framed not as an afterthought but as a predictable sequela, would demonstrate depth. The checklist’s aesthetic-clean, minimalist-fails to convey the gritty reality of daily vigilance required by patients. One must also lament the omission of practical strategies for dining out, such as leveraging gluten‑free certification programs or establishing communication protocols with restaurant staff. The reference to “oral rehydration solutions” would have been richer with a mention of specific electrolyte ratios endorsed by the WHO. Finally, the call for “regular follow‑ups” should be quantified: suggest a timeline of serological testing at six months, then annually, to monitor tTG‑IgA trends. In sum, while the piece offers a veneer of helpfulness, it falls short of the scholarly rigor and compassionate empathy that the suffering celiac community deserves.
Audrin De Waal
November 26, 2025 AT 01:46People love to act like gluten is some mythic beast, but it’s just a protein that decides who gets to eat pizza. If you’re not paying attention, it’ll sneak into your life like a covert philosopher, questioning everything you thought you knew about food. Stay sharp, challenge the hidden gluten, and you’ll keep the gut peace.