How to Involve Family or Caregivers in Medication Support
 Nov, 24 2025
Nov, 24 2025
When someone you love is taking multiple medications, it’s easy to assume they’re managing it all on their own. But the truth is, medication adherence is one of the biggest challenges in home healthcare-especially for older adults or people with chronic conditions. Nearly half of all people don’t take their meds as prescribed. And when that happens, it doesn’t just mean a pill gets missed-it means trips to the ER, hospital stays, and sometimes even preventable deaths. The good news? Involving family or caregivers isn’t just helpful-it’s one of the most effective ways to keep someone safe and healthy at home.
Start with a Complete Medication List
Before you do anything else, sit down and make a full, up-to-date list of every medication. Not just the big ones. Not just the ones you remember. Every pill, patch, inhaler, injection, and liquid. Include the brand name, generic name, exact dose (like "Lisinopril 10mg"), how often it’s taken ("once daily at 8 AM"), and why it’s being taken ("for high blood pressure"). Don’t forget over-the-counter drugs, vitamins, and supplements-those can interact just like prescription meds.The Agency for Healthcare Research and Quality says this list needs 17 specific details per medication. That sounds like a lot, but it’s the difference between catching a dangerous interaction and missing it. One caregiver in Ohio found out her mother’s new blood pressure med was reacting badly with her arthritis drug-only because she had the full list and showed it to the pharmacist. That kind of mistake can kill. Update this list within 24 hours of any change, whether it’s a new prescription, a dose tweak, or a drug being stopped. Keep a printed copy in your wallet and another in a binder at home. Share it with every doctor, pharmacist, and caregiver involved.
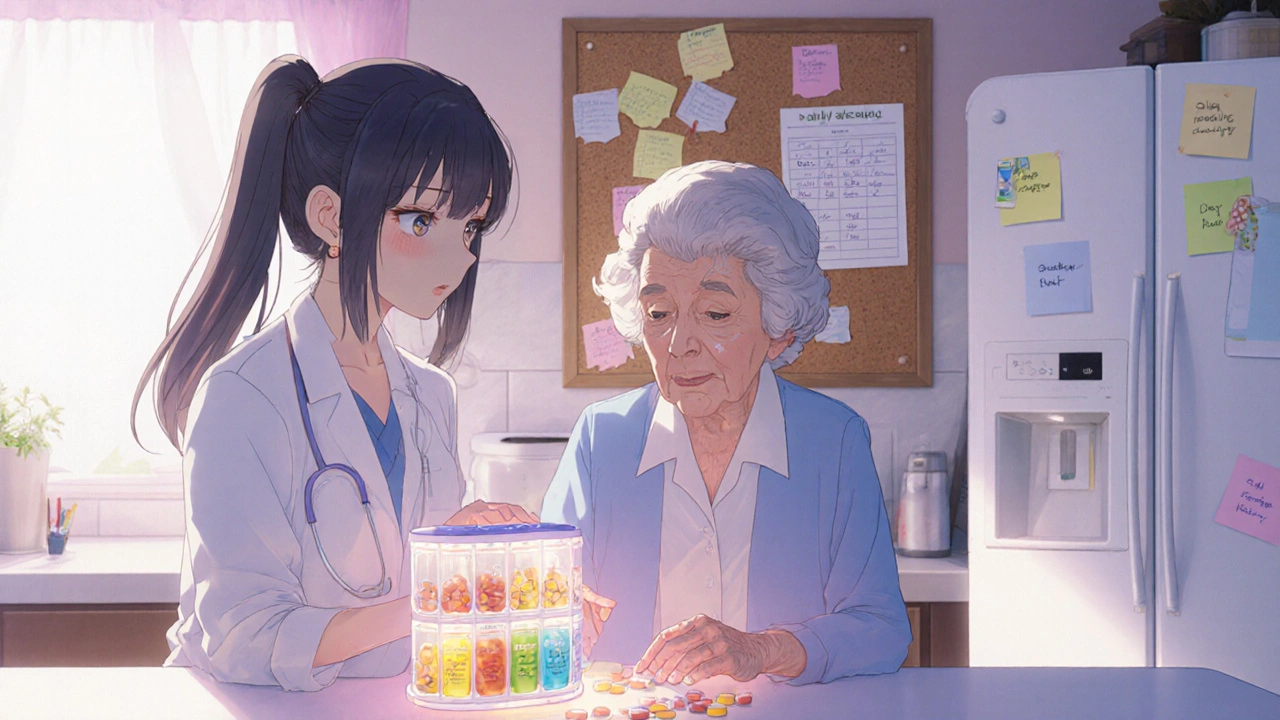
Use a Pill Organizer-But Choose the Right One
A simple 7-day pill box with morning and evening compartments reduces missed doses by 37%, according to a 2022 study in the Journal of the American Geriatrics Society. But not all organizers are equal. If someone needs meds three or four times a day, a basic box won’t cut it. Look for ones with alarms, or better yet, electronic dispensers like Hero Health or MedMinder. These devices lock and unlock at the right time, play voice reminders, and even send alerts to your phone if a dose is skipped.One study found these smart dispensers cut missed doses by 62%. That’s huge. But don’t just buy one and hope it works. Set it up with the person you’re helping. Make sure they understand how it beeps, how to open it, and what to do if it doesn’t release a pill. If they have memory issues, the alarm alone won’t be enough-they need someone nearby to check in.
Build Medication Routines Into Daily Life
People don’t remember to take pills because they’re busy, tired, or distracted. But they remember brushing their teeth, eating breakfast, or watching the news. That’s why linking meds to existing habits-called "habit stacking"-works so well. The National Institute on Aging recommends tying each medication to a daily routine. Take your blood pressure pill right after you brush your teeth. Take your diabetes meds before lunch. Take your nighttime painkiller right before you turn off the TV.This isn’t just a trick-it’s science. A 2022 study showed habit stacking improved adherence by 28%. The brain starts to associate the action with the behavior. Over time, the pill becomes part of the ritual, not an extra chore. Write the routine down on a sticky note next to the toothbrush or the coffee maker. Use the same phrase every time: "After I eat breakfast, I take my statin." Repetition builds memory.
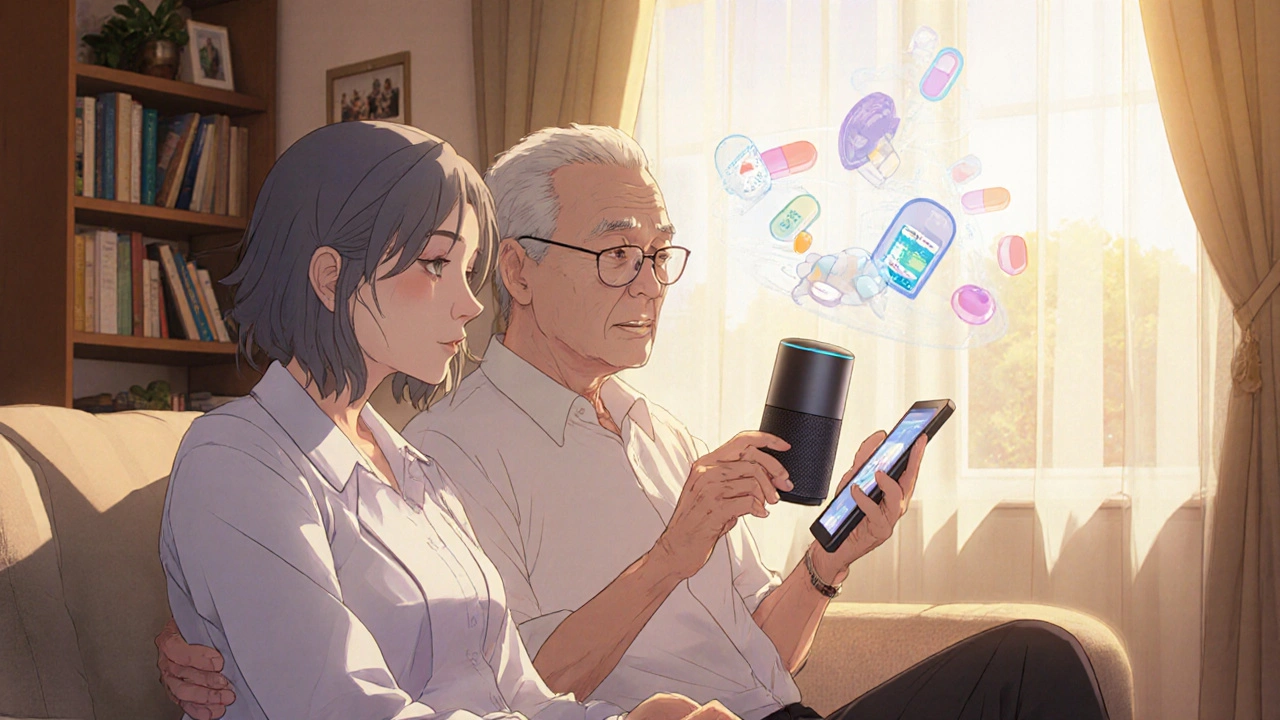
Set Up Digital Reminders and Voice Helpers
Phones are everywhere. So are voice assistants. Use them. Apps like Medisafe or Round Health let you schedule reminders, track doses, and even notify family members if a pill is missed. In clinical trials, users saw a 45% improvement in adherence compared to paper logs.For people with dementia or vision problems, voice assistants like Amazon Alexa or Google Home are game-changers. Ask, "Alexa, remind me to take my warfarin at 7 PM," and it will. A 2023 University of Pittsburgh study found voice reminders reduced missed doses by 37% in patients with cognitive decline. You can even set up Alexa Care Hub to send alerts to your phone if your parent doesn’t respond to a reminder. It’s not surveillance-it’s safety.
Know When to Call the Pharmacist
Pharmacists are the most accessible medication experts in the healthcare system. Ninety-two percent of U.S. pharmacies have a pharmacist on-site without an appointment. And they’re trained to spot dangerous interactions, confusing labels, and unnecessary meds.When you pick up a new prescription, don’t just walk away. Ask these four questions:
- When should this be taken-before, during, or after food?
- Are there any foods, drinks, or other meds I should avoid?
- What should I do if I miss a dose?
- How long until I start to feel the effect?
Don’t be shy. Pharmacists expect these questions. In fact, the American Pharmacists Association says caregivers who ask these questions reduce adverse events by 40%. If something doesn’t make sense-like a pill that looks different than last time-ask. It could be a different generic, or worse, a mistake.
Do Quarterly Medication Reviews
Medications pile up. Someone sees a cardiologist, then a rheumatologist, then a pain specialist. Each one adds a new drug. No one stops to ask: "Do we still need all of these?" That’s called polypharmacy-and it’s dangerous. Nearly half of adults over 65 take five or more medications. That increases their risk of falls by 50% and hospitalization by 30%.Every three months, sit down with the person you’re helping and go through every med. Use the American Geriatrics Society’s Beers Criteria-a list of 30 drugs that are risky for older adults. Is there a sleeping pill that causes confusion? A muscle relaxer that makes them dizzy? A blood thinner that interacts with a new supplement? Bring the full list to the doctor. Ask: "Can any of these be stopped?" A 2022 study showed quarterly reviews cut inappropriate prescriptions by 22%.
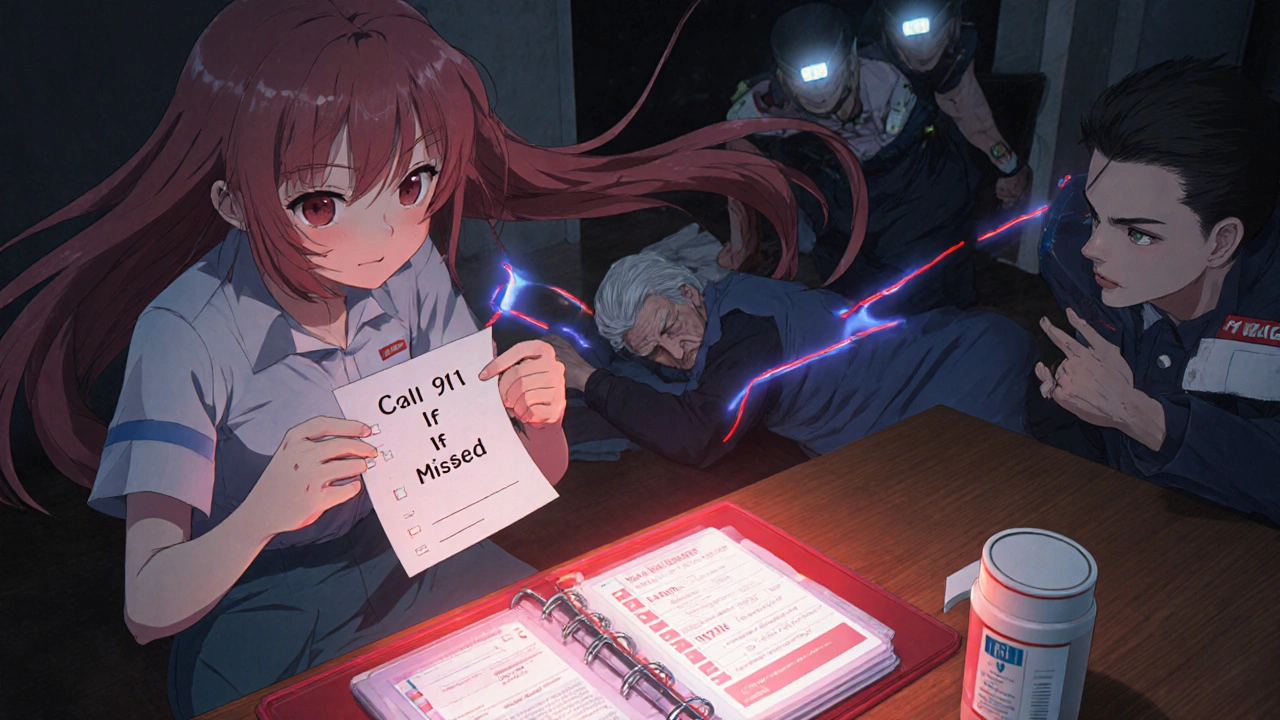
Prepare for Emergencies
Not all missed doses are equal. Missing a vitamin? Maybe not a big deal. Missing insulin? Anticoagulants like warfarin? That’s an emergency. Create a "medication red list"-a simple note on the fridge or in the wallet that says: "If these are missed, call 911 or go to the ER." Include: insulin, blood thinners, seizure meds, heart meds like beta-blockers, and steroids like prednisone.Also, keep a printed emergency contact sheet: your name, phone, doctor’s name, pharmacy, and all meds. Put it in the front of the binder. If the person falls, has a stroke, or gets confused, first responders need this info fast. A 2023 study in the Annals of Internal Medicine found families who used a red list cut emergency visits by 19%.
Attend Appointments Together
Doctors don’t always know what’s happening at home. They see a patient for 15 minutes. They don’t see the pill organizer with half-empty compartments. They don’t hear the cough that started after the new antibiotic. They don’t know the patient skipped doses because the pills cost too much.Go to every appointment. Sit next to the person. Take notes. Ask questions. The AARP found that 89% of caregivers who attended appointments understood the medication plan better-and 76% of those using digital apps reported fewer missed doses. You’re not just a helper. You’re a co-manager of care. And your voice matters.
Watch for Burnout
Medication management is exhausting. It’s constant. It’s stressful. It’s emotional. The National Alliance for Caregiving found 42% of caregivers say managing meds is their most stressful task. If you’re feeling overwhelmed, you’re not alone. And you don’t have to do it all.Ask for help. Split the tasks. One person handles pharmacy pickups. Another sets up the pill organizer. Someone else calls for refills. Use community resources. Medicare Part D offers free Medication Therapy Management (MTM) for people taking eight or more drugs. CVS and Walgreens now have dedicated caregiver support lines. Local Area Agencies on Aging often provide free medication reviews. You’re not failing if you ask for support-you’re being smart.
Know the System Is Changing
The system is finally catching up. Since 2018, hospitals have been required to include caregivers in discharge planning. By 2025, all electronic health records must include patient-facing medication lists. Medicare’s MTM program served over 11 million people in 2023. Digital tools are growing fast-Alexa Care Hub usage jumped 200% last year. AI-powered medication assistants are coming. This isn’t just about you doing more. It’s about the system finally supporting you.But right now, you’re the bridge between the doctor’s office and the medicine cabinet. You’re the one who notices the tremor after a new pill. You’re the one who remembers the refill date. You’re the one who catches the mistake before it becomes a crisis. That’s not just helpful. It’s lifesaving.

Erika Hunt
November 24, 2025 AT 22:40So many people overlook how crucial it is to document every single thing-prescription, OTC, supplement, even that herbal tea Grandpa swears by for his ‘joint pain’… I’ve seen families lose loved ones because someone forgot to mention the turmeric capsules interacting with warfarin. It’s not paranoia, it’s precision. Write it down. Print it. Laminated if you have to. And update it like you update your phone’s OS-constantly.
Also, the pill organizers with alarms? Life-changing. My aunt used to forget her meds twice a day. Got her a MedMinder. Now she gets a voice reminder, a light flash, and a text to me if she skips. She calls it her ‘robot nurse.’ I call it peace of mind.
Sharley Agarwal
November 25, 2025 AT 01:59This is why Western families fail. Too much tech. Too little presence.
giselle kate
November 26, 2025 AT 04:41Of course you need to involve family-what, you think the government’s gonna do it? We’re the last line of defense. America’s healthcare system is a joke. Pills cost more than rent. Doctors don’t listen. So who’s gonna sit there at 7 AM with your grandma, making sure she swallows her blood thinner? You. Me. Us. No one else. Stop outsourcing your moral duty to robots and apps.
And don’t get me started on those ‘smart’ dispensers. They’re nice, sure. But if your parent can’t open the damn thing because their hands shake, what’s the point? Tech doesn’t replace love. It just pretends to.
My dad’s on 14 meds. I print the list. I go to every appointment. I call the pharmacy every time a new script comes in. I don’t care if it’s ‘not my job.’ It’s my dad. And if you think someone else should do it, you’re not ready to be family.
Stop scrolling. Start showing up.
prasad gaude
November 27, 2025 AT 17:54In India, we don’t have pill organizers or Alexa reminders. We have mothers who wake up at 5 AM to boil water for medicine. We have siblings who swap shifts so one can sleep. We have aunts who memorize every pill’s color and shape because the labels fade. We don’t need tech-we need tradition.
But here’s the truth: tech can help. Not replace. Help. I’ve seen my cousin in Delhi use Medisafe to remind his diabetic uncle. It worked. Why? Because the family still sat with him. The phone just made sure they didn’t forget.
Westerners think automation fixes everything. We know: love fixes everything. Tech just reminds you to show up.
Kimberley Chronicle
November 28, 2025 AT 12:20Excellent framework-particularly the emphasis on polypharmacy audits via the Beers Criteria. The clinical utility of quarterly medication reviews is empirically validated, with a 22% reduction in inappropriate prescribing (per JAMA Internal Medicine, 2022). Moreover, integrating MTM services under Medicare Part D represents a high-impact, low-cost intervention that mitigates ADEs by 38% in multimorbid elderly populations.
That said, the behavioral economics of adherence suggests that habit-stacking leverages intrinsic reward pathways via dopamine reinforcement-hence the 28% adherence boost. Recommend pairing this with implementation intention scripting: ‘If X happens, then I will do Y.’
Also, consider deploying AI-driven NLP tools to parse medication lists from free-text EHR notes. Currently underutilized.
Shirou Spade
November 28, 2025 AT 19:18It’s funny how we treat medicine like a checklist when it’s actually a relationship. Every pill has a story. Every dose has a fear. Every missed tablet has a silence behind it.
We fix the system. But who fixes the loneliness that makes people skip their meds because they don’t want to be a burden? That’s the real crisis.
Lisa Odence
November 30, 2025 AT 03:11OMG YES!!! 🙌 I literally printed 3 copies of my mom’s med list and put one in her purse, one on the fridge with magnets, and one in my phone’s notes with a notification set to remind me to check it every Sunday! 💯 And I use Medisafe with alerts to my phone AND my sister’s phone!! 📱❤️ We even made a color-coded chart for her pills-red = dangerous, green = safe, yellow = ask the pharmacist!! 🎨 I’m basically a medication ninja now 😎
Also, my pharmacist gave me a free pill splitter and a little booklet on interactions. I cried. She’s my hero. 💕
Pallab Dasgupta
November 30, 2025 AT 08:17You think this is hard? Try doing this in a village in Bihar where the nearest pharmacy is 40 km away, the power goes out every night, and your mother’s insulin has to be kept cool in a clay pot filled with wet sand.
Yes, Alexa helps. But what helps more? A son who walks 5 km every morning to buy the meds. A daughter who learns to read the label in English because the doctor’s handwriting is garbage. A neighbor who shares her fridge.
Technology is a tool. But human connection? That’s the medicine.
fiona collins
November 30, 2025 AT 14:23Respectful boundaries matter. Not everyone wants to be monitored. Not everyone wants reminders. Ask before you act.
Emily Craig
December 1, 2025 AT 16:45Oh wow so we’re supposed to be full-time pharmacists now? Thanks for the 2000-word essay on how to be a perfect caregiver without once mentioning that most of us are working 60-hour weeks, raising kids, and can’t afford to take time off. You make it sound like we’re volunteers. We’re not. We’re drowning.
And yeah, I know I should’ve made a list. But I was too busy crying in the car after my mom yelled at me because I forgot to refill her blood pressure med. Again.
So thanks for the guilt trip, Karen. I’ll just go back to feeling like a failure.
Karen Willie
December 2, 2025 AT 08:25To Emily-thank you for saying that. I’ve been there. You’re not alone. And you’re not failing. You’re human.
One of my friends told me: ‘You don’t have to do it all. You just have to do what you can today.’ So I started small. I set one reminder. I wrote one med down. I asked one question at the pharmacy.
That’s enough.
You’re doing better than you think.