Hashimoto's Thyroiditis: Understanding Autoimmune Thyroid Disease and How to Manage TSH Levels
 Jan, 6 2026
Jan, 6 2026
Hashimoto's thyroiditis isn't just another thyroid problem. It's the most common reason people in places like the U.S., Canada, and Western Europe end up with an underactive thyroid. And it's not something that just shows up overnight. It creeps in-slowly, quietly-until your energy drops, your weight creeps up, and you start feeling like you're always cold, even in summer. If you’ve been told your TSH is high but you’re not sure what that really means, you’re not alone. Most people don’t understand why their doctor keeps asking for blood tests every few months or why their medication dose keeps changing. This isn’t guesswork. It’s science. And it’s personal.
What Exactly Is Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis is an autoimmune disease. That means your immune system, which is supposed to protect you from viruses and bacteria, turns against your own thyroid gland. It starts attacking the cells that make thyroid hormones. Over time, this destroys the gland’s ability to produce enough hormone. The result? Hypothyroidism. By the time most people get diagnosed, up to 80% of their thyroid tissue may already be damaged.
The disease was first described in 1912 by a Japanese doctor named Hakaru Hashimoto. Back then, it was called struma lymphomatosa. Today, we know it affects about 1-2% of the general population-but in women over 50, that number jumps to 5-10%. Women are ten times more likely to develop it than men. Why? It’s not just hormones. Genetics play a big role. If you have a family member with Hashimoto’s, lupus, type 1 diabetes, or rheumatoid arthritis, your risk goes up.
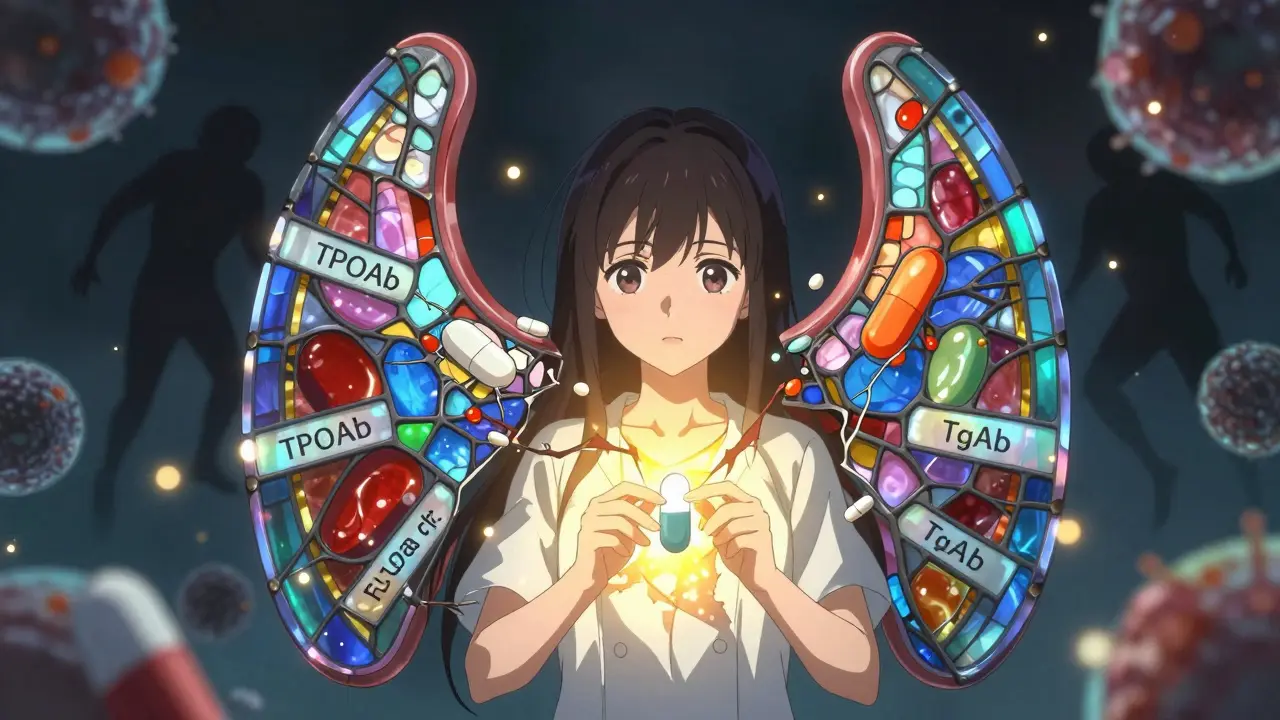
The immune attack shows up in blood tests as two main antibodies: thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb). Over 90% of people with Hashimoto’s have high TPOAb. That’s the most reliable marker. If your TSH is high and your TPOAb is positive, you’ve got Hashimoto’s. No biopsy needed.
How Does Hashimoto’s Progress?
It doesn’t happen all at once. There are four clear stages:
- Phase 1: Euthyroid with antibodies-Your thyroid still works fine, your TSH is normal, but your antibodies are already up. You might feel fine, or you might have mild fatigue or brain fog. This stage can last years.
- Phase 2: Subclinical hypothyroidism-Your TSH starts creeping up, usually between 4.5 and 10 mIU/L. Your free T4 is still normal. Many doctors wait here before prescribing medication. But if you’re symptomatic, treatment may help.
- Phase 3: Overt hypothyroidism-TSH is above 10 mIU/L, and your free T4 drops. This is when symptoms get real: weight gain, dry skin, constipation, depression, heavy periods, hair loss. Most people get diagnosed here.
- Phase 4: Atrophy-The thyroid shrinks. The goiter (swelling) that once made your neck look swollen disappears. But the damage is permanent. You’ll need lifelong medication.
And here’s something few doctors mention: about 15-20% of people go through a brief phase called hashitoxicosis. Your thyroid gets so inflamed it leaks out stored hormone, causing temporary hyperthyroidism. You might feel anxious, have heart palpitations, lose weight, or feel sweaty-even though you later develop full-blown hypothyroidism. It’s confusing, scary, and often misdiagnosed as Graves’ disease.
Why TSH Is the Cornerstone of Management
TSH-thyroid-stimulating hormone-is the body’s main signal for thyroid function. It’s made by the pituitary gland. When your thyroid isn’t making enough hormone, your pituitary screams louder: “Make more!” So TSH rises. That’s why doctors test it first.
But here’s the catch: TSH alone isn’t always enough. In 5-10% of Hashimoto’s cases, antibodies interfere with the TSH test, making it look higher than it really is. That’s why free T4 must be checked too, especially if you still feel awful despite a “normal” TSH.
So what’s the right TSH target? It depends on you.
- Adults under 60: Aim for 1.0-2.5 mIU/L. This range reduces fatigue, brain fog, and weight gain.
- Adults over 60-70: 2.5-4.5 mIU/L is safer. Going too low increases heart rhythm problems and bone loss.
- Pregnant women: Below 2.5 mIU/L in the first trimester. Above that, miscarriage risk jumps 2.3 times. Many endocrinologists target 1.0-2.0 mIU/L during pregnancy.
- People with heart disease: Don’t push TSH too low. Even 2.0-3.0 may be too aggressive.
These aren’t arbitrary numbers. They’re based on large studies tracking symptoms, heart health, and quality of life. The American Thyroid Association and European Thyroid Association both agree: one-size-fits-all doesn’t work.

Levothyroxine: The Standard Treatment
Levothyroxine (T4) is the gold standard. It’s a synthetic version of the hormone your thyroid used to make. It’s cheap, stable, and effective for 85-90% of people.
But dosing is tricky. You don’t take it and feel better the next day. It takes 4-6 weeks for your body to fully adjust. That’s why you need blood tests every 6-8 weeks after a dose change. Too fast, and you risk heart palpitations or bone thinning. Too slow, and you suffer longer than necessary.
Here’s how it works in practice:
- Start with 12.5-25 mcg if you’re over 60 or have heart issues.
- For younger, healthy adults: 1.6 mcg per kg of body weight is the starting point.
- Adjust by 12.5-25 mcg at a time. Never jump by 50 mcg unless under close supervision.
- Take it on an empty stomach, 30-60 minutes before breakfast. Coffee, calcium, iron, and soy can block absorption.
And yes-brand matters. The FDA says levothyroxine has a narrow therapeutic index. That means even small differences in how the drug is made can affect your levels. If you switch from Synthroid to a generic, get your TSH checked in 6-8 weeks. Many patients need a dose adjustment.
Why Some People Still Feel Bad on Levothyroxine
Here’s the hard truth: 10-15% of people on levothyroxine still have symptoms-fatigue, depression, brain fog, muscle pain-even with a “normal” TSH. Why?
Some experts believe the body can’t convert enough T4 to T3, the active hormone. That’s led some to try T3 (liothyronine) or combination therapy. But the science doesn’t support it for most. A 2017 meta-analysis of 87 studies found no consistent benefit from adding T3. The American Association of Clinical Endocrinologists says: don’t use it routinely.
But here’s what does help:
- Timing and consistency: Take your pill at the same time every day. Even a 2-hour shift can affect absorption.
- Avoid biotin: Biotin supplements (common in hair and nail formulas) can cause false TSH readings-up to 30% error. Stop them 3 days before blood tests.
- Seasonal changes: TSH levels rise 15-20% in winter. If you’re stable in summer but feel off in January, your dose may need a small winter boost.
- Weight changes: Gain 10 pounds? You might need more medication. Lose 10? You might need less.
And stress? It’s huge. Chronic stress raises cortisol, which blocks T4-to-T3 conversion. That’s why so many patients say their symptoms flare during divorce, job loss, or illness.
Real People, Real Struggles
On Reddit’s r/Hashimotos community, 57% of 1,892 users say their TSH fluctuates even with perfect dosing. Common triggers? Gluten (32%), stress (41%), and seasonal shifts (27%). One woman wrote: “I was on 100 mcg for 3 years. Then I got sick with the flu. My TSH jumped from 1.8 to 7.2 in 6 weeks. I didn’t change anything-just got sick.”
Another patient said: “I thought I was doing everything right. But I was taking my pill with my morning coffee. Once I switched to water only, my TSH dropped from 4.8 to 1.9 in 8 weeks.”
And then there’s the emotional toll. One survey found 68% of patients needed three or more dose changes before they felt normal. That’s frustrating. It’s not you. It’s the disease. It’s unpredictable.
What’s Next? The Future of Hashimoto’s Management
Levothyroxine isn’t going anywhere. But research is shifting. Scientists are now looking at the immune system itself. In 2022, a study in Nature Medicine found that 25% of treatment-resistant Hashimoto’s patients have antibodies that block TSH receptors-something thought to only happen in Graves’ disease. That could mean new drugs down the line.
Twelve clinical trials are now testing drugs that calm down the T-cells attacking the thyroid. If they work, we might one day stop just replacing hormone and start stopping the attack.
By 2030, genetic testing may tell us who needs lower TSH targets based on their CTLA-4 or PTPN22 genes. Personalized medicine is coming.
For now? Stick with the basics: consistent dosing, proper testing, and patience. Your TSH is your guide. But your symptoms? They’re your compass. If you feel off, speak up. Don’t accept “your numbers are fine” if you’re still exhausted.
What to Do Next
If you have Hashimoto’s:
- Get your TSH and free T4 tested every 6-8 weeks after a dose change.
- Test in the morning, before taking your pill, and before eating or drinking anything except water.
- Stop biotin supplements 3 days before blood work.
- Take levothyroxine on an empty stomach, at least 30 minutes before breakfast.
- Don’t take calcium, iron, or soy within 4 hours of your pill.
- Keep a symptom journal. Note fatigue, mood, weight, and sleep. Bring it to every appointment.
- Ask for a free T3 test if you’re still symptomatic despite normal TSH.
If you’re newly diagnosed: Give it time. It can take 6-12 months to find your sweet spot. You’re not failing. Your body is adjusting.
And remember: Hashimoto’s isn’t your fault. It’s not caused by sugar, stress, or bad habits. It’s genetics and immune misfire. You didn’t break it. You’re managing it. And that’s enough.
Can Hashimoto’s thyroiditis be cured?
No, Hashimoto’s cannot be cured. The immune system continues to attack the thyroid, and the damage is permanent. However, it can be fully managed with levothyroxine. Once your TSH is in the right range, most people live normal, healthy lives without symptoms. The goal isn’t to reverse the disease-it’s to replace what your thyroid can no longer make.
Do I need to avoid gluten if I have Hashimoto’s?
Not everyone. But about 5-10% of people with Hashimoto’s also have celiac disease, and many more report feeling better on a gluten-free diet. If you suspect gluten is triggering your symptoms, try eliminating it for 3 months and track your energy, digestion, and lab results. It’s not a cure, but it can reduce inflammation and antibody levels in sensitive individuals. Always test for celiac first with a blood test (tTG-IgA).
Why does my TSH keep changing even though I take my pill every day?
Many factors affect TSH: weight changes, seasonal variations (higher in winter), stress, illness, medications like iron or calcium, and even sleep patterns. Your body’s demand for thyroid hormone isn’t static. That’s why regular testing is essential. A change in dose doesn’t mean you’re doing something wrong-it means your body is adapting.
Can I stop taking levothyroxine if I feel better?
No. Once your thyroid is destroyed by Hashimoto’s, it won’t recover. Stopping medication will cause your TSH to rise again, and symptoms will return-often worse than before. Levothyroxine isn’t addictive. It’s simply replacing a hormone your body no longer produces. You need it for life.
Is it safe to take levothyroxine long-term?
Yes, when taken at the correct dose. Long-term studies show no increased risk of heart disease or osteoporosis if your TSH is kept in the target range. The real danger is under-treatment-low hormone levels raise cholesterol, increase heart disease risk, and worsen depression. Properly dosed levothyroxine is one of the safest and most effective medications in medicine.
Should I get my thyroid antibodies tested every year?
No. Once you’ve been diagnosed, antibody levels don’t need routine monitoring. They don’t predict how you’ll feel or how fast your thyroid will fail. TSH and free T4 are the only tests that matter for managing your treatment. Antibodies are useful for diagnosis, not ongoing care.

Elen Pihlap
January 8, 2026 AT 04:03i just took my pill with coffee and now i feel like a zombie who forgot how to breathe. why does everyone act like this is easy??
Emma Addison Thomas
January 8, 2026 AT 15:52Interesting how the article mentions seasonal TSH shifts. In the UK, we see this too-winter fatigue is real, and it’s not just ‘being lazy.’ I’ve learned to adjust my dose quietly, without making a fuss. Doctors rarely mention it.
Anastasia Novak
January 10, 2026 AT 01:39OMG. I’ve been on levothyroxine for 7 years and I swear my doctor doesn’t even read my labs. Last month I was at 3.8 and felt like I was drowning in concrete. They said ‘it’s fine’ and I nearly cried in the parking lot. This isn’t medicine-it’s guesswork with a clipboard. And don’t get me started on biotin. I took it for ‘glow skin’ and my TSH looked like a horror movie. I’m never trusting another supplement again.
Jonathan Larson
January 11, 2026 AT 02:10The physiological and immunological complexity of Hashimoto’s underscores the necessity of individualized therapeutic approaches. While levothyroxine remains the cornerstone of treatment, the interplay between cortisol, T4-to-T3 conversion, and immune dysregulation necessitates a systems-based understanding rather than a reductionist reliance on TSH alone. The data supporting TSH targets within the 1.0–2.5 mIU/L range for younger adults is robust, yet clinical judgment must account for comorbidities, age, and patient-reported outcomes. The absence of routine antibody monitoring is evidence-based, but patient education remains critically underprioritized in primary care.
Alex Danner
January 12, 2026 AT 09:28My TSH went from 8.2 to 1.9 after I stopped taking my pill with my protein shake. I thought I was doing everything right-until I read that calcium and soy block absorption. Now I take it at 5am with water and I feel like a new person. No magic. Just basic science. Why do so many people skip this stuff?
Sai Ganesh
January 14, 2026 AT 07:50In India, many patients don’t even get tested properly. We have to pay out of pocket for free T4. TSH is the only test doctors check. I had to travel 300km to find someone who knew about TPOAb. Hashimoto’s is not rare here-it’s just ignored.
Paul Mason
January 16, 2026 AT 04:46Gluten-free? Please. I tried it for three months and my energy didn’t change. If you’re not celiac, stop listening to influencers. Your thyroid isn’t broken because you ate bread. Take your pill and move on.
Katrina Morris
January 18, 2026 AT 04:14i just found out my tsh jumped after i got sick and i was like wow maybe this isnt all in my head? also i take my pill right when i wake up and i dont even drink water first because i forget and i still feel better than i did 2 years ago so maybe im doing something right??
Anthony Capunong
January 19, 2026 AT 18:04Why are we letting foreigners tell us how to treat our own bodies? In America, we have the best doctors and the best meds. If you’re still tired after levothyroxine, maybe you’re just weak. Stop blaming the disease and start lifting weights.
Ayodeji Williams
January 21, 2026 AT 05:01bro the thyroid is just a gland… why are we making it a cult?? 😂 i took my pill once and forgot for 2 weeks… still alive. maybe we’re all just stressed and need to chill the f*** out 🤷♂️
Kyle King
January 22, 2026 AT 08:55They’re hiding the truth. Levothyroxine is just a cover-up. The real cure is iodine and colloidal silver. The FDA and Big Pharma don’t want you to know. Your TSH isn’t high-it’s being manipulated by fluoride in the water. I’ve reversed mine with bentonite clay and moonlight. You’re being lied to.
Kamlesh Chauhan
January 23, 2026 AT 19:41all this talk about tsh and antibodies but no one talks about the fact that you need to sleep 9 hours and drink 3 liters of water and never ever eat sugar or else you die. duh.
Mina Murray
January 24, 2026 AT 15:59Actually, the American Thyroid Association updated their guidelines in 2023 and they now recommend TSH under 2.0 for ALL adults under 70, not just under 60. You’re citing outdated info. And no, you don’t need to test antibodies yearly-unless you’re pregnant or have a family history of other autoimmune diseases. Also, your doctor should check reverse T3 if you’re still symptomatic. Most don’t even know what that is.
Rachel Steward
January 26, 2026 AT 02:27Let’s be real: Hashimoto’s isn’t a disease-it’s a metaphor. Your thyroid is a mirror of your unprocessed trauma, your suppressed rage, your fear of being seen. The antibodies? They’re your soul screaming for boundaries. Levothyroxine just numbs the signal. You want to heal? Stop taking the pill. Start journaling. Walk barefoot on the earth. Burn your gluten. Your body isn’t broken-it’s begging you to wake up.
Emma Addison Thomas
January 26, 2026 AT 20:57Interesting how the article mentions seasonal TSH shifts. In the UK, we see this too-winter fatigue is real, and it’s not just ‘being lazy.’ I’ve learned to adjust my dose quietly, without making a fuss. Doctors rarely mention it.
Jonathan Larson
January 27, 2026 AT 03:34Your observation about seasonal variation aligns with the circadian and photoperiodic regulation of thyroid function. The hypothalamic-pituitary-thyroid axis is sensitive to ambient light and temperature, which explains the winter elevation in TSH. This is not a flaw in treatment-it is a physiological adaptation. The challenge lies in translating this biological rhythm into clinical practice, which remains underdeveloped in most primary care settings.