Genetics of Gallstones: How Your Genes Influence Risk
 Oct, 12 2025
Oct, 12 2025
Gallstone Risk Calculator
This tool estimates your risk of developing gallstones based on factors discussed in the article. Your risk is influenced by genetics, family history, and lifestyle choices.
Did you know that up to 25% of the adult population will develop gallstones at some point, and that genetics can explain a sizable chunk of those cases? If you’ve ever wondered why gallstones run in families, you’re about to get the answers you need.
Key Takeaways
- Specific gene variants (e.g., ABCG5 and ABCG8) raise cholesterol saturation in bile, making stones more likely.
- Family history is a strong predictor, but lifestyle still matters - the two work together.
- Genetic testing can pinpoint high‑risk individuals, helping clinicians tailor diet, medication, and monitoring plans.
- Even with a genetic predisposition, simple changes-weight control, balanced diet, regular ultrasound-can keep stones at bay.
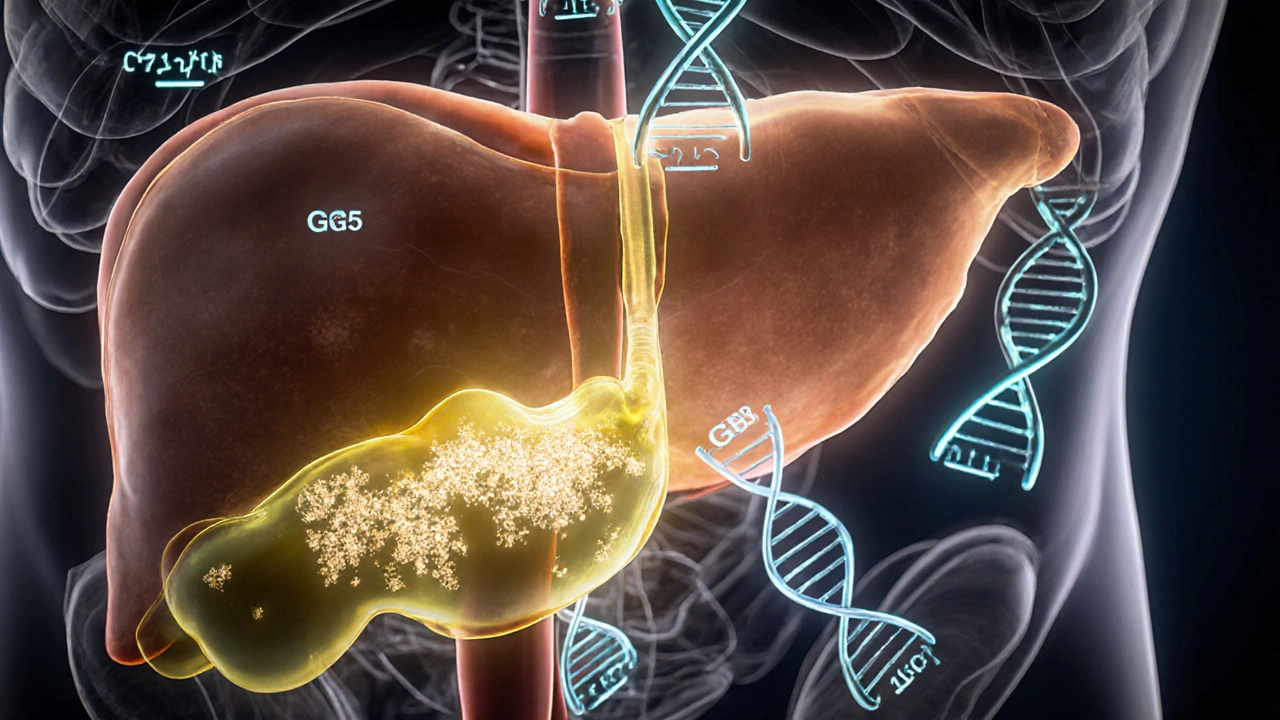
What Are Gallstones?
Gallstones are solid particles that form in the gallbladder, a small organ tucked under the liver that stores bile. The two main types are:
- Cholesterol gallstones - hard, yellow‑white stones made mostly of hardened cholesterol.
- Pigment gallstones - darker stones formed from excess bilirubin, often linked to hemolysis or liver disease.
Both types share a common pathway: bile becomes supersaturated, and crystals nucleate, grow, and eventually lodge in the gallbladder.
How Genetics Drive Gallstone Formation
Research over the past decade shows that several genes regulate bile composition, cholesterol metabolism, and gallbladder motility. Variants that tip the balance toward supersaturation raise stone risk even when diet or weight are optimal.
Most of the hereditary influence follows an autosomal‑dominant pattern with incomplete penetrance - meaning you can carry a risky gene without ever developing stones, especially if you keep other risk factors low.

Major Genetic Variants Linked to Gallstones
The most consistently replicated genes are:
- ABCG5 - encodes a transporter that pumps cholesterol into bile. A common missense variant (D19H) increases cholesterol output by ~15%.
- ABCG8 - partners with ABCG5; together they form a heterodimer. The T400K variant amplifies the effect of ABCG5, leading to doubly high biliary cholesterol.
- ABCB4 - moves phosphatidylcholine into bile, protecting cholesterol crystals. Loss‑of‑function mutations create a phospholipid‑deficient bile that crystallizes more easily.
- CYP7A1 - the rate‑limiting enzyme in converting cholesterol to bile acids. The -203A>C promoter polymorphism reduces enzyme activity, leaving more cholesterol in the pool.
- SLCO1B1 - a liver transporter influencing statin clearance. Certain alleles raise plasma cholesterol, indirectly feeding the gallbladder.
Each variant adds a modest risk (odds ratios 1.2‑1.8), but when several stack together, the cumulative risk can double or triple.
Gene‑Environment Interaction: Why Lifestyle Still Matters
Even the most “high‑risk” genotype can be mitigated by diet and weight control. For example, a study of 8,000 New Zealand adults found that carriers of the ABCG5‑D19H allele who maintained a BMI<25 had a stone incidence similar to non‑carriers. In contrast, obese carriers faced a 3‑fold increase.
Key environmental modifiers include:
- High‑fat, low‑fiber diets that increase cholesterol secretion into bile.
- Rapid weight loss (e.g., after bariatric surgery) that oversaturates bile with cholesterol.
- Hormonal factors - estrogen therapy and pregnancy raise cholesterol levels in bile, especially risky for genetically predisposed women.
Assessing Your Genetic Risk
Two practical ways to gauge risk:
- Family History - if a first‑degree relative (parent, sibling, child) had gallstones before age50, your odds rise by ~1.5×.
- Genetic Testing - commercial panels (e.g., 23andMe, Myriad) now include ABCG5, ABCG8, and ABCB4. A targeted‘Gallstone Risk Panel’ costs roughly $150‑$250 and returns a risk score based on allele count.
Clinicians may also order a fasting lipid panel and a liver function test to see if biochemical markers align with genetic findings.

Prevention Strategies Tailored to Your Genes
Once you know your risk, you can personalize prevention:
- Dietary tweaks - increase soluble fiber ( oats, beans ), limit saturated fat (<30g/day), and add omega‑3 rich foods (salmon, flaxseed) to lower biliary cholesterol.
- Weight management - aim for gradual weight loss (0.5‑1kg/week) if overweight; rapid drops can actually trigger stones.
- Medication options - Ursodeoxycholic acid (UDCA) can dissolve cholesterol crystals and is especially helpful for ABCB4 mutation carriers.
- Regular monitoring - a yearly abdominal ultrasound catches silent stones early, allowing non‑surgical management.
For people with strong ABCG5/ABCG8 variants, some clinicians prescribe low‑dose statins to curb hepatic cholesterol synthesis, indirectly reducing bile saturation.
Genetic vs. Lifestyle Risk Factors: A Quick Comparison
| Factor | Typical Impact (Odds Ratio) | Modifiability | Action Steps |
|---|---|---|---|
| ABCG5/D19H Variant | 1.4‑1.6 | Low (cannot change genes) | Targeted diet, UDCA, statin if indicated |
| ABCB4 Loss‑of‑Function | 2.0‑2.5 | Low | UDCA, monitor liver enzymes, avoid high‑fat meals |
| Obesity (BMI>30) | 1.8‑2.2 | High | Gradual weight loss, exercise, calorie control |
| High‑fat, low‑fiber diet | 1.5‑1.9 | High | Increase fiber, replace saturated fats with unsaturated fats |
| Rapid weight loss (>10%/month) | 2.3‑3.0 | Medium (manage pace) | Plan weight loss over ≥6 months, use medical supervision |
Frequently Asked Questions
Can I get gallstones if I have no family history?
Yes. Lifestyle factors like obesity, high‑fat diets, and certain medications can cause stones on their own. Genetics raises the odds, but it’s not a prerequisite.
Should I get genetic testing if I’ve never had gallstones?
Testing is most useful if you have a strong family history or other risk factors. It can guide preventive measures, but it isn’t necessary for everyone.
Do medications like statins affect gallstone risk?
Some studies suggest low‑dose statins lower biliary cholesterol, modestly reducing stone formation, especially in carriers of cholesterol‑transport genes.
How often should I have an ultrasound if I’m genetically high‑risk?
Annual scans are a good rule of thumb. If you develop symptoms or have a rapid weight‑loss plan, increase the frequency to every 6months.
Is there any cure for gallstones without surgery?
Ursodeoxycholic acid can dissolve small cholesterol stones over months to years, but it works best when the stone burden is low and the patient adheres to the regimen.
Next Steps & Troubleshooting
If you suspect a genetic component, start with a simple pedigree: jot down any relatives with gallstones, their ages, and whether they required surgery. Bring this chart to your GP or gastroenterologist.
Common hurdles:
- Insurance denies genetic testing. - Ask for a “medical necessity” letter that cites your family history and the potential to avoid costly surgery.
- Positive test but no symptoms. - Begin lifestyle changes immediately; consider a baseline ultrasound and schedule follow‑ups.
- Side effects from UDCA. - Start with a low dose, take it with meals, and monitor liver enzymes after 4‑6 weeks.
Remember, genetics loads the dice, but you control the roll. By combining the right diet, steady weight management, and targeted medical monitoring, you can keep gallstones at arm’s length.

Edward Morrow
October 12, 2025 AT 04:37Listen up, folks-if your lineage is riddled with gallstones, you might as well brace for a rocky ride. Cut the greasy junk, swap fries for veggies, and maybe the Almighty will cut you some slack. Your genes aren’t a death sentence if you hustle hard enough.
Shayne Tremblay
October 18, 2025 AT 06:29Hey everyone! This piece is a solid boost for anyone wanting to take charge of their health. Knowing your genetic odds is the first step toward crushing those stone threats. Keep moving, eat balanced, and stay positive-you’ve got this!
Stephen Richter
October 24, 2025 AT 08:21I must point out that the risk calculator lacks peer‑reviewed validation. Additionally, it omits critical factors such as diabetes or hyperlipidemia.
Musa Bwanali
October 30, 2025 AT 09:14You’re on the right track, Stephen, but don’t let the numbers intimidate you. Adjust your diet, stay active, and you’ll outsmart the odds.
Allison Sprague
November 5, 2025 AT 11:06The article does a decent job of laying out the basic genetic contributors to gallstone formation.
However, it glosses over the profound impact of epigenetic modifiers, which can swing risk scores dramatically.
For instance, the interaction between cholesterol metabolism genes and high‑fat diets is far more nuanced than a simple additive score.
Your mother’s gallstones may signal a hereditary predisposition, but without considering lifestyle, the prediction is weak.
Moreover, the calculator assumes a linear relationship between BMI and risk, ignoring the threshold effects observed in clinical cohorts.
I also noticed the gender weighting is overly simplistic-female hormones do more than just add a point.
The omission of hormonal contraceptive use is a glaring oversight.
From a methodological standpoint, the scoring rubric lacks transparency; readers deserve to see the raw data.
Without confidence intervals, the risk levels feel like guesswork rather than evidence‑based medicine.
Nevertheless, the tool can still spark valuable conversations with patients about preventive measures.
Encouraging a low‑fat, high‑fiber diet remains the cornerstone of stone prevention.
Regular physical activity not only trims BMI but also improves gallbladder motility.
Hydration is another underrated factor-adequate water intake dilutes bile and reduces crystallization.
Genetic counseling may be appropriate for families with multiple affected members, especially when considering bariatric surgery.
Ultimately, while the calculator is a nice introductory aid, clinicians should integrate it with comprehensive risk assessments.
Take the tool with a grain of salt and always verify findings against current guidelines.
leo calzoni
November 11, 2025 AT 12:58Honestly, most of you are clueless about basic genetics. If you can’t grasp a simple inheritance pattern, you’re not fit to discuss gallstones. Stop whining and actually read the literature.
KaCee Weber
November 17, 2025 AT 14:50While I respect your passion, dear leo, I must point out that dismissing others as 'clueless' does little to foster constructive dialogue. 🌱 In fact, the interplay between diet, ethnicity, and genetic variants is a tapestry worth exploring with curiosity rather than contempt. Your straightforward tone could be softened with a touch of empathy, especially for readers navigating complex health information. Let’s celebrate diverse perspectives and invite collaboration, because science thrives on shared inquiry. 😊
jess belcher
November 23, 2025 AT 16:42Gallstone risk isn’t set in stone; cultural eating habits play a huge role, and simple swaps can make a world of difference.
Sophia Simone
November 29, 2025 AT 18:34While I appreciate the enthusiasm, it must be noted that attributing gallstone prevalence solely to diet overlooks the substantial genetic heterogeneity observed across populations. Therefore, the presented calculator, though user‑friendly, may inadvertently mislead users by downplaying complex polygenic interactions.
Juan Sarmiento
December 5, 2025 AT 20:26Great discussion, everyone! Remember, consistency is key-stay active, keep your meals balanced, and don’t let a single high‑fat day undo your progress. You’ve got the power to steer your health in the right direction.
Cindy Knox
December 11, 2025 AT 22:18Absolutely, Juan. Your reminder hits home-small daily choices stack up, and the body rewards steady, mindful habits more than occasional extremes.
beverly judge
December 18, 2025 AT 00:10For those seeking a deeper dive, consider reviewing recent meta‑analyses on ABCG8 and SLCO1B1 variants; they provide nuanced insights beyond the basic calculator and can guide personalized dietary recommendations.
Capt Jack Sparrow
December 24, 2025 AT 02:02Nice tool.
Manju priya
December 30, 2025 AT 03:37Absolutely love the emphasis on genetics, Beverly! 🌟 By combining genetic insights with a balanced diet and regular exercise, anyone can reduce their gallstone risk significantly. Keep shining that knowledge, and let’s empower more people together! 💪😊