Deprescribing Frameworks: How to Safely Reduce Medications and Cut Side Effects
 Feb, 14 2026
Feb, 14 2026
Medication Review Tool
Identify Potential Inappropriate Medications
This tool helps you identify medications that might be unnecessary for older adults based on the 2023 Beers Criteria guidelines. Please note: This is for educational purposes only and does not replace professional medical advice.
Every year, millions of older adults take more medications than they need. Some of these drugs were prescribed years ago for a condition that’s since improved-or never really existed in the first place. The result? A cluttered medicine cabinet, more side effects, and a higher risk of hospital visits. This isn’t just a problem-it’s a widespread, under-addressed crisis. Deprescribing is the solution: a structured, patient-centered way to stop unnecessary medications and reduce harm. It’s not about cutting pills randomly. It’s about thinking critically, listening closely, and acting deliberately.
What Exactly Is Deprescribing?
Deprescribing isn’t stopping meds because they’re old or expensive. It’s a clinical process that asks: Are the risks of this drug still outweighing the benefits? For older adults, especially those with multiple health issues, taking five or more medications (polypharmacy) increases the chance of falls, confusion, kidney damage, and dangerous drug interactions. The World Health Organization estimates that 40% of older adults globally are on potentially inappropriate medications. In the U.S., one in three hospital admissions among seniors is linked to medication problems. Deprescribing flips the script: instead of adding more drugs to manage side effects, we remove the ones causing them.
The concept became formalized around 2012, led by researchers in Canada who created the first evidence-based guidelines. Today, deprescribing.org is the go-to resource, offering clear, step-by-step protocols for five major drug classes: proton-pump inhibitors (PPIs), benzodiazepines, antipsychotics, antihyperglycemics, and opioids. Each guideline includes specific criteria, tapering schedules, and monitoring steps-no guesswork.
How Deprescribing Works: The 4-Step Process
Successful deprescribing follows a clear, repeatable pattern. It’s not a one-time decision. It’s a conversation that unfolds over weeks or months.
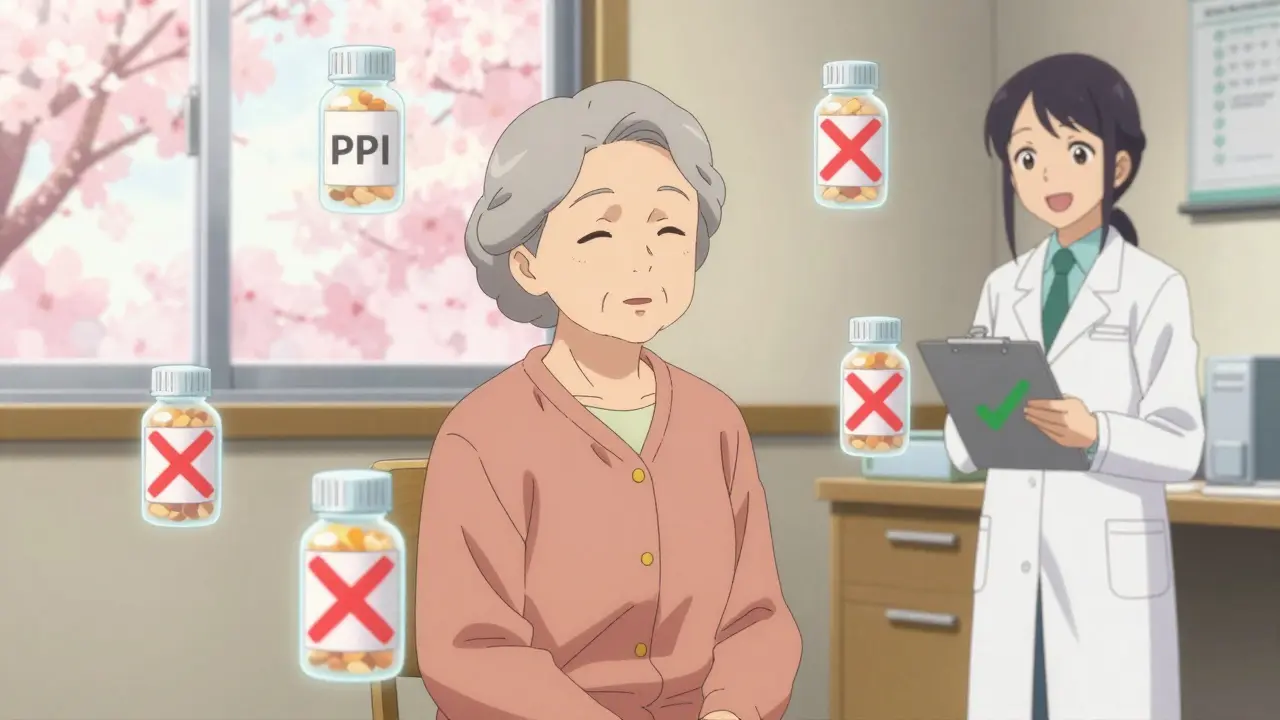
- Identify candidates-Look for drugs with known risks in older adults. The 2023 Beers Criteria lists 34 potentially inappropriate medications, including long-term PPIs (used for heartburn), sleeping pills like zolpidem, and antipsychotics prescribed for dementia-related agitation.
- Evaluate benefit vs. harm-Ask: Is this drug still helping? Is the patient’s life expectancy shortening? Are they experiencing dizziness, fatigue, or memory lapses? A 2023 JAMA study found that 62% of seniors on long-term PPIs had no documented reason for continued use.
- Plan the taper-Never stop cold turkey. Benzodiazepines, for example, require gradual reduction over 4-12 weeks to avoid rebound anxiety or seizures. PPIs may cause temporary acid rebound, so switching to as-needed use before stopping is key.
- Monitor and adjust-Check in after 2, 4, and 8 weeks. Did their sleep improve? Did their blood pressure drop? Did they have fewer falls? If symptoms return, reassess. Sometimes the drug was helping more than we thought.
The Shed-MEDS framework, validated in a 2023 clinical trial with 372 older adults, showed patients dropped an average of 1.8 medications without increased hospital visits. That’s not luck-it’s protocol.
Who Should Lead Deprescribing?
Pharmacists are the unsung heroes of deprescribing. In settings where pharmacists are part of the care team, medication reduction rates jump by 35-40%. Why? They have the time. They know drug interactions. They can walk patients through tapering schedules and explain withdrawal symptoms before they happen.
But in most U.S. primary care clinics, doctors see patients for an average of 7.2 minutes per visit. There’s no time to review 12 medications, discuss goals of care, or address fears about stopping “something I’ve taken for 20 years.” That’s why successful programs have pharmacist-led clinics, nurse practitioners trained in medication management, and electronic health record (EHR) alerts that flag high-risk prescriptions.
One study found that clinics using EHR prompts-where doctors must actively choose to prescribe a high-risk drug instead of it being auto-filled-reduced inappropriate prescribing by 41%. Technology helps, but human judgment still leads.

What Medications Are Most Often Deprescribed?
Not all drugs are equal. Some have clear, safe pathways to stop. Others don’t. Here are the top five, based on evidence from deprescribing.org and the American Geriatrics Society:
- Proton-pump inhibitors (PPIs)-Used for heartburn. Most people only need them for 4-8 weeks. Yet 70% of long-term users have no diagnosis justifying continued use. Tapering over 4-8 weeks reduces rebound acid by 85%.
- Benzodiazepines and BZRAs-Sleep aids like lorazepam or zolpidem. These increase fall risk by 50% in older adults. Tapering over 8-12 weeks cuts withdrawal symptoms to under 10% of cases.
- Antipsychotics-Often prescribed off-label for dementia-related behaviors. These drugs increase stroke risk and death. Guidelines recommend stopping unless there’s clear psychosis. Non-drug approaches (music therapy, routine changes) work better long-term.
- Antihyperglycemics-Diabetes meds like sulfonylureas. In frail seniors, low blood sugar is more dangerous than high sugar. Switching to metformin or stopping entirely improves safety without worsening A1C.
- Opioids-For chronic non-cancer pain. Many patients are on doses higher than needed. Tapering by 10% per month reduces overdose risk and improves alertness.
These five classes account for over 70% of all deprescribing opportunities. But here’s the gap: there are no clear guidelines for 500+ other medication combinations. That’s why some clinicians hesitate.
Why Don’t More Doctors Do It?
Two big barriers: time and fear.
Most doctors aren’t trained in deprescribing. Medical schools focus on prescribing, not stopping. And when a patient says, “I’ve been on this pill since 1998,” it’s hard to say, “Let’s stop it.” Patients worry about withdrawal, rebound symptoms, or losing a sense of security. A 2022 study found 22% of seniors felt anxious about stopping even one medication.
Meanwhile, clinics lack the tools. Only 32% of U.S. healthcare systems have EHR systems that support deprescribing workflows. And only 28% of primary care practices have formal protocols-compared to 63% in Canada, where national guidelines have been in place since 2018.
But the tide is turning. In June 2024, the American Medical Association adopted its first policy urging physicians to routinely review all medications. Starting in 2026, Medicare will include deprescribing metrics in physician pay ratings. The NIH is funding AI tools to scan EHRs and flag candidates for deprescribing. By 2030, experts predict these checks will be as routine as checking blood pressure.
What Patients Need to Know
If you’re on multiple medications, ask:
- “Is this still necessary?”
- “What happens if I stop it?”
- “Are there non-drug options?”
- “Can we try reducing the dose first?”
Most people who stop unnecessary meds report feeling better: more energy, clearer thinking, fewer stomach issues, and less confusion. One 81-year-old woman in a 2022 study stopped three sleeping pills and a muscle relaxant. Within three weeks, she stopped falling. She said, “I feel like I got my life back.”
But not everyone should stop. For some, a medication may be the only thing keeping them comfortable-especially in advanced dementia or end-of-life care. Deprescribing isn’t one-size-fits-all. It’s personalized. It’s about aligning meds with what matters to you.
The Bottom Line
Deprescribing isn’t about taking away medicine. It’s about restoring balance. Too many pills can be as dangerous as too few. The goal isn’t to be pill-free-it’s to be right-pill-free. With clear guidelines, trained teams, and better tools, we can cut side effects, prevent hospital stays, and help older adults live better-not just longer.
It’s time to stop thinking of deprescribing as risky. It’s time to see it for what it is: the most responsible form of prescribing.
Is deprescribing safe for older adults?
Yes, when done properly. A 2023 JAMA Internal Medicine trial of 372 older adults found no increase in hospitalizations or deaths after reducing medications. In fact, patients had fewer falls and better alertness. The key is gradual tapering, close monitoring, and involving a pharmacist or trained clinician. Stopping cold turkey or without a plan is risky-but that’s not deprescribing. That’s random discontinuation.
Can I stop my medications on my own?
No. Some medications, like benzodiazepines, antipsychotics, or high-dose opioids, can cause dangerous withdrawal symptoms if stopped suddenly. Others, like blood pressure or diabetes drugs, may need adjustments to avoid rebound effects. Always talk to your doctor or pharmacist before changing anything. They can create a safe, personalized plan.
What if I’m scared to stop a medication I’ve taken for years?
That fear is normal-and valid. Many patients feel like their meds are a safety net. The best approach is to start small. Try reducing one pill at a time, with clear goals: “Let’s see if you feel less dizzy after stopping this sleep aid.” Track symptoms. Celebrate improvements. Most people find that after a few weeks, they feel better than they did on the pills.
Do I need a pharmacist to help with deprescribing?
You don’t absolutely need one, but you’ll have a much higher success rate if you do. Pharmacists are trained to spot unnecessary or harmful meds, know how to taper safely, and can communicate clearly with doctors. In studies, deprescribing success rates are 35-40% higher when pharmacists are involved. If your clinic doesn’t have one, ask your doctor to refer you to a medication therapy management program.
Are there tools I can use to check if I’m on too many meds?
Yes. The Beers Criteria (updated in 2023) and STOPP/START v3 are free, evidence-based tools used by clinicians worldwide. You can search them online or ask your pharmacist for a copy. Also, deprescribing.org offers downloadable algorithms for common drug classes. These aren’t meant to replace your doctor-but they’re great conversation starters.

Michael Page
February 15, 2026 AT 22:06Deprescribing isn't just a medical protocol-it's a philosophical reckoning with our obsession over control. We prescribe to feel like we're doing something, even when the body has already moved on. The real crisis isn't polypharmacy; it's the illusion that more intervention equals better care. We've turned medicine into a ritual, not a science. The data doesn't lie: 62% of long-term PPI users have no documented indication. That's not clinical practice. That's inertia dressed as care.
And yet, we're still surprised when patients fall, get confused, or end up in the ER. We built the system to reward prescribing, not pausing. The system doesn't break because of bad actors-it breaks because of silent, systemic complacency.
Joe Grushkin
February 16, 2026 AT 02:53Pharmacists leading deprescribing? Please. The real problem is doctors being replaced by algorithm-driven middlemen. You think a pharmacist who's never seen a patient's full history can decide whether someone needs their blood pressure med? That's not care-that's outsourcing responsibility to people who don't even have a license to diagnose.
And don't get me started on that Shed-MEDS study. 372 patients? That's a lab experiment. Real medicine happens in 7-minute visits with 80-year-olds who don't care about guidelines-they care about not feeling like they're being abandoned by their own doctor.
Virginia Kimball
February 17, 2026 AT 10:02I love this so much. I’ve watched my mom go from 12 pills a day to 4-and she’s got more energy than she had in years. No more dizziness, no more confusion, no more midnight bathroom trips because of a ‘heartburn’ pill she didn’t even need.
It’s not about taking meds away. It’s about giving people back their lives. That 81-year-old woman who stopped falling? That’s the win. That’s the reason we do this. We’re not removing safety nets-we’re replacing tangled, outdated ones with ones that actually hold you up.
And yes, pharmacists are heroes. They’re the ones who notice the duplicate prescriptions, the dangerous combos, the meds that’ve been on autopilot since Clinton was president. We need more of them in clinics, not less.
Daniel Dover
February 18, 2026 AT 16:39Clear guidelines save lives. Pharmacist involvement doubles success rates. Simple.
Chiruvella Pardha Krishna
February 20, 2026 AT 10:14The West has forgotten that medicine was once a practice of restraint. We now treat the body like a machine that needs constant lubrication. Deprescribing is the return to the wisdom of the ancients: sometimes, the best treatment is nothing at all. The overprescribing epidemic is not a failure of knowledge-it is a failure of humility.
Modern medicine worships intervention. But nature heals. The body remembers balance. When we strip away the unnecessary, the body often restores itself. We are not curing-we are interfering. Deprescribing is the quiet rebellion against this arrogance.
Kaye Alcaraz
February 20, 2026 AT 10:31Deprescribing is not about reducing pills. It is about restoring agency. Patients are not passive recipients of protocols. They are partners in their own health. The fact that 22% of seniors fear stopping a medication reveals a deeper truth: we have failed to communicate, to educate, to listen.
Every taper should begin with a conversation-not a checklist. Every decision should be rooted in the patient’s values, not the algorithm’s output. The EHR alerts? Helpful. The pharmacist? Essential. But the human connection? Irreplaceable.
We must train clinicians not just to stop prescribing-but to start listening.
Sarah Barrett
February 21, 2026 AT 16:24Interesting how the article frames deprescribing as a revolution. It’s not. It’s just good medicine. If a drug was prescribed 20 years ago for a condition that no longer exists, why are we still giving it? That’s not stubbornness-it’s negligence.
And yet, we call it ‘risk’ to stop. That’s absurd. The real risk is continuing a regimen that’s been obsolete for a decade. I’ve seen patients on three different anticholinergics for ‘sleep’ and ‘anxiety’ and ‘digestion’-all of which were causing their confusion. Stop one, and the others become irrelevant.
Clarity, not complexity, is the goal.
Erica Banatao Darilag
February 22, 2026 AT 07:05i just wanted to say thank you for writing this. my dad was on 11 meds and we had no idea half of them were even still needed. we found out after a hospital stay that he was on a muscle relaxant for a back issue he’d had 15 years ago. he stopped it and his energy came back. he said he felt like he could breathe again.
the scary part? his doctor didn’t even think to ask. we had to push for it. i hope this becomes standard. not because of guidelines-but because we finally start seeing people, not charts.
Kapil Verma
February 22, 2026 AT 11:46Western medicine is collapsing under its own weight. You think America is the leader in healthcare? Look at the data-40% of seniors on inappropriate meds, 1 in 3 hospitalizations from drugs. This isn’t innovation. This is corruption. Pharma lobbies write the guidelines. Doctors are paid by volume, not outcomes. And now you want to hand deprescribing to pharmacists? That’s just moving the deck chairs.
Real change starts with dismantling the profit-driven model. Until then, this is just a PR stunt dressed in clinical language.
Mandeep Singh
February 23, 2026 AT 07:57Everyone’s talking about deprescribing like it’s some breakthrough. Newsflash: we’ve known this for decades. In India, elders have been stopping meds naturally for generations-not because of guidelines, but because they lived with less, trusted their bodies, and didn’t let doctors turn them into pill factories. We didn’t need EHR alerts or Shed-MEDS. We had common sense.
Now you want to export this as a ‘Western innovation’? Please. The truth is, the West is finally catching up to what traditional cultures never forgot: sometimes, less is more. And it’s not about tools-it’s about humility. We stopped listening. Now we’re pretending we invented the solution.
Betty Kirby
February 23, 2026 AT 15:36This is the most dangerous narrative I’ve seen in years. You’re telling people to stop medications without understanding their full history. What about the patient who’s on a beta-blocker because they had a silent MI? Or the one on an anticoagulant after a pulmonary embolism? You think a pharmacist scanning an EHR can catch that? No. Only a doctor who knows the patient’s story can.
And don’t get me started on the ‘non-drug options’ for dementia agitation. Music therapy? That’s cute. But when someone’s screaming at 3 a.m., hitting staff, and trying to climb out the window-what’s your alternative? A hug? A playlist?
This isn’t progress. It’s recklessness with a pretty acronym.
Michael Page
February 24, 2026 AT 02:56Of course, the real issue isn’t the medications-it’s the system that makes them necessary. We don’t have a deprescribing crisis. We have a primary care collapse. Doctors see 30 patients a day. No time for reviews. No reimbursement for conversations. No incentive to question a prescription written by someone else five years ago.
So we patch. We add. We keep the pills because stopping them requires more work than starting them.
Pharmacists can’t fix this alone. We need structural change. Not just protocols. We need time. We need payment reform. We need to stop treating medicine like a conveyor belt.