Cleocin Gel vs Other Acne Treatments: Clindamycin Comparison
 Oct, 16 2025
Oct, 16 2025
Acne Treatment Decision Guide
Let's find your best acne treatment
Answer these brief questions to get personalized recommendations for your skin concerns.
1. What type of acne do you have?
2. How sensitive is your skin?
3. How long have you been treating acne?
4. Are you concerned about antibiotic resistance?
5. Do you have specific skin concerns?
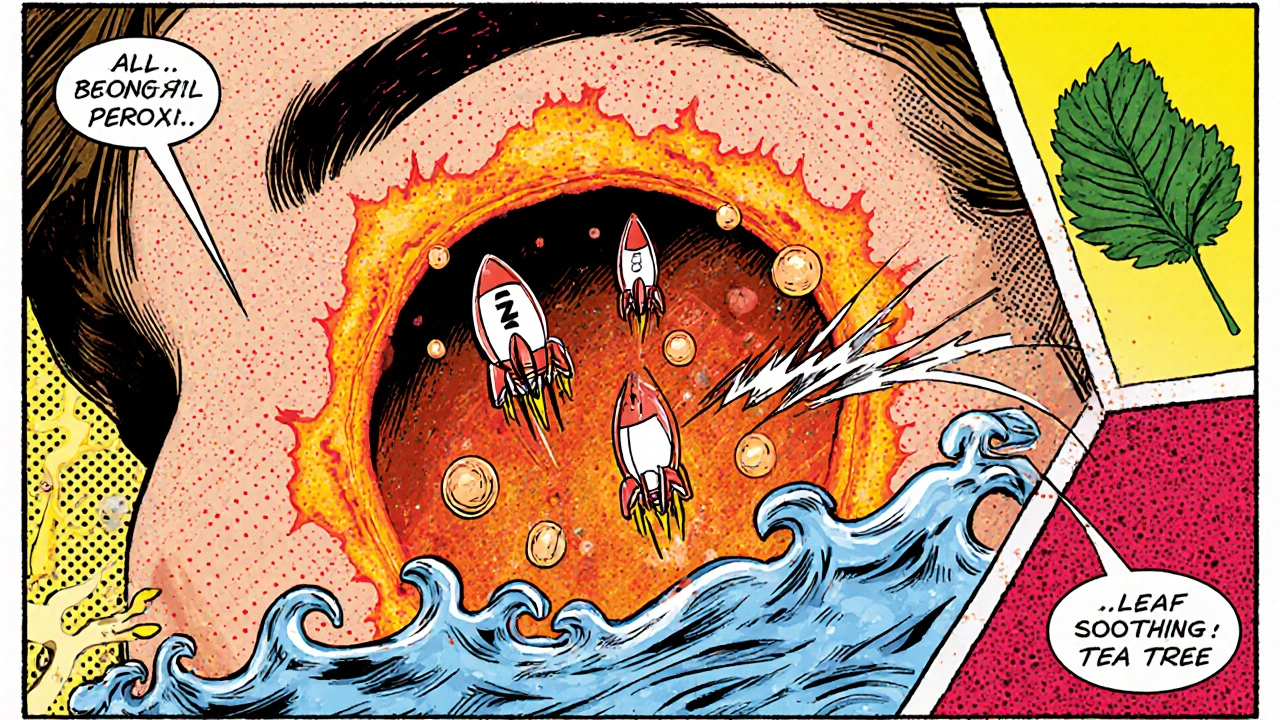
When you’re battling persistent acne, picking the right topical can feel like a guessing game. One of the most prescribed options is Cleocin Gel - a 1% clindamycin gel that targets the bacteria behind breakouts while calming inflammation.
How Cleocin Gel Works
Clindamycin belongs to the lincosamide family of antibiotics. It interferes with bacterial protein synthesis, effectively stopping Propionibacterium acnes the primary acne‑causing microbe from multiplying. At the same time, the gel base delivers a mild anti‑inflammatory effect, reducing redness and swelling.
Key Benefits & Drawbacks of Cleocin Gel
- Targeted action: Works directly on the skin, limiting systemic exposure.
- Low risk of severe irritation compared with retinoids.
- Convenient once‑daily application.
- May develop bacterial resistance if used long‑term without rotation.
- Can cause mild dryness, itching, or a temporary burning sensation.
Popular Alternatives Overview
Below is a quick snapshot of the most common acne medications that clinicians pair with or substitute for clindamycin.
- Benzoyl Peroxide - a potent oxidizing agent that kills acne bacteria and helps unclog pores.
- Erythromycin - a macrolide antibiotic similar to clindamycin but with a different resistance profile.
- Tretinoin - a prescription‑strength retinoid that speeds up cell turnover and clears clogged follicles.
- Doxycycline - an oral tetracycline antibiotic used for moderate to severe inflammatory acne.
- Tea Tree Oil - a natural essential oil with antibacterial properties, often used in over‑the‑counter gels.
- Salicylic Acid - a beta‑hydroxy acid that exfoliates inside the pore and reduces sebum buildup.
- Azelaic Acid - a dicarboxylic acid that kills P. acnes, reduces keratin production, and brightens post‑inflammatory marks.
Comparison Table
| Medication | Active Ingredient | Formulation | Typical Use | Pros | Cons |
|---|---|---|---|---|---|
| Cleocin Gel | Clindamycin 1% | Topical gel | Daily on affected areas | Targets bacteria, minimal irritation | Potential resistance, mild dryness |
| Benzoyl Peroxide | 2.5-10% | Gel, cream, wash | 2-3× daily | Fast antibacterial action, reduces oil | Can bleach fabrics, cause peeling |
| Erythromycin | Erythromycin 2% | Topical gel/cream | Once or twice daily | Effective against P. acnes, well‑tolerated | Resistance comparable to clindamycin |
| Tretinoin | Tretinoin 0.025-0.1% | Cream or gel | Nightly | Prevents comedones, improves texture | Initial irritation, photosensitivity |
| Doxycycline | Doxycycline 100mg | Oral tablet | Once daily (or split dose) | Works systemically, reduces deep inflammation | GI upset, photosensitivity, requires prescription |
| Tea Tree Oil | Melaleuca alternifolia oil 5-10% | Topical gel/solution | 2× daily | Natural option, mild antibacterial | Potential allergic reactions, less potent |
| Salicylic Acid | 0.5-2% | Leave‑on pads, gels | Once or twice daily | Exfoliates inside pore, reduces blackheads | Can cause dryness, not ideal for very sensitive skin |
| Azelaic Acid | 15-20% | Cream or gel | Twice daily | Anti‑bacterial, brightens hyperpigmentation | Mild tingling, slower results |
Choosing the Right Treatment - Decision Guide
Not every acne breakout needs a prescription. Use the following quick checklist to decide whether Cleocin Gel or another option fits your skin.
- Inflammatory vs. non‑inflammatory: If lesions are red, pustular, or cystic, an antibiotic (Cleocin, erythromycin, doxycycline) adds value.
- Risk of resistance: Rotate clindamycin with benzoyl peroxide or a retinoid after 8‑12 weeks.
- Skin sensitivity: Sensitive users may favor azelaic acid or low‑percentage salicylic acid over benzoyl peroxide.
- Convenience: Topicals require daily commitment; oral doxycycline is handy for busy schedules but needs a prescription.
- Budget: Over‑the‑counter options like tea tree oil are cheaper but often slower.
How to Use Topical Treatments Safely
Even the best medication can backfire if you don’t apply it right. Follow these universal tips:
- Cleanse gently with a non‑scrubbing cleanser 15minutes before application.
- Pat skin dry; excess moisture dilutes gels and creams.
- Apply a thin layer-no more than a pea‑size amount per affected zone.
- Allow each product to dry for at least 5minutes before layering another.
- Start with once‑daily use; increase to twice‑daily only if tolerated.
- Use a non‑comedogenic moisturizer to combat dryness.
- Never share prescription products; bacterial resistance can spread.
Frequently Asked Questions
Can I use Cleocin Gel together with benzoyl peroxide?
Yes. Combining a topical antibiotic with benzoyl peroxide reduces the chance of resistance and improves overall bacterial kill rate. Apply benzoyl peroxide in the morning, wait it to dry, then use Cleocin Gel at night.
How long does it take to see results with Cleocin Gel?
Most patients notice reduced redness within 2-3 weeks, but noticeable lesion clearance often requires 8-12 weeks of consistent use.
Is clindamycin safe during pregnancy?
Clindamycin is classified as Category B by the FDA, meaning animal studies show no risk and there are no well‑controlled human studies. Doctors may still prefer a non‑antibiotic option unless acne is severe.
What should I do if I develop a rash while using Cleocin Gel?
Stop the gel immediately and rinse the area with cool water. If the rash persists or spreads, contact your dermatologist for an alternative regimen.
Are there effective over‑the‑counter alternatives to clindamycin?
Tea tree oil, salicylic acid, and azelaic acid provide mild antibacterial and exfoliating effects without a prescription. They work best for mild to moderate acne and can be combined with a retinoid for added benefit.

Jeremy Laporte
October 16, 2025 AT 14:03Hey folks, great rundown on the options! I’ve found Cleocin works pretty well when I keep it simple and use a light moisturizer. Just be sure to start slow so your skin doesn’t get too dry, that’s what trippd me up at first. If you’re worried about resistance, pair it with a low‑strength benzoyl peroxide every other day. Hope this helps anyone navigating the acne maze!
Patricia Hicks
October 17, 2025 AT 12:16I just wanted to share a little bit of my own journey because sometimes the science feels a bit sterile without the human context. When I first tried Cleocin Gel, I was skeptical about a simple antibiotic gel being enough for my stubborn hormonal breakouts. I started by cleansing with a gentle, sulfate‑free cleanser, waited about fifteen minutes, and then dabbed a pea‑size amount on each blemish. Within a week I noticed the red halos around my papules soften, which was encouraging but not yet a miracle. By week three the count of active pustules dropped noticeably, and the occasional lingering spot began to fade. I made sure to pair the gel with a low‑dose benzoyl peroxide in the mornings, because the literature warns about resistance if you use antibiotics alone for too long. My dermatologist also recommended a non‑comedogenic moisturizer with ceramides to counteract the mild dryness I felt after the first few applications. I kept a simple log, noting any itching, burning, or new lesions, and was relieved to see only minimal irritation. Around the eight‑week mark, most of my inflammatory lesions were gone, and the overall texture of my skin felt smoother. I did experience a brief flare when I missed a night’s dose, which reminded me how consistent dosing really matters. The only downside I found was the cost; a month’s supply can be pricey compared to over‑the‑counter options, but I judge it worth it for the results. If you have oily skin, you might want to add a gentle salicylic acid pad a few times a week to keep the pores clear. For those with very sensitive skin, start with every other night and gradually increase frequency as tolerated. In my experience, rotating off the antibiotic after about three months with a retinoid helped maintain the improvements without a rebound. Overall, I’d say Cleocin Gel is a solid backbone in an acne regimen, especially when you respect the guidelines and monitor your skin’s response. Hope this long‑winded share gives some practical insight beyond the textbook description.
Quiana Huff
October 18, 2025 AT 10:30Yo fam, diving into the mech‑of‑action: clindamycin inhibits the 50S ribosomal subunit, essentially halting P. acnes protein synthesis, which is why you see that rapid reduction in inflammatory cytokine cascade 😊. Compared to a broad‑spectrum BPO oxidative burst, the antibiotic’s MIC is lower, so you get a cleaner therapeutic index. If you stack with a low‑potency retinoid, you’ll engage both keratinocyte differentiation pathways and the innate immune response. Just remember to monitor for potential C. difficile colonization if you ever switch to oral doxy for severe cases!
William Nonnemacher
October 19, 2025 AT 08:43Cleocin is overpriced and barely better than generic benzoyl peroxide.
Alex Ramos
October 20, 2025 AT 06:56Jeremy, you raise some solid points, however, the claim that a “light moisturizer” suffices is overly simplistic; many patients with barrier‑impaired skin will still experience transepidermal water loss despite such measures, and the clinical literature backs this up. Moreover, the suggestion to pair with “low‑strength” benzoyl peroxide neglects the fact that sub‑therapeutic concentrations may actually promote bacterial resistance-something dermatologists caution against. It would be prudent to specify exact percentages, for instance 2.5% BPO applied once nightly, followed by a 15‑minute absorption window before Cleocin; this protocol has been shown to maximize bactericidal synergy. In addition, the role of adjunctive non‑comedogenic moisturizers containing niacinamide cannot be overstated, as they simultaneously modulate inflammatory mediators. Lastly, patient education on adherence is paramount-without consistent use, even the most evidence‑based regimen will falter.
Matthew Platts
October 21, 2025 AT 05:10Hey, I kinda echo Pat’s approach; letting the gel work for 8‑12 weeks before expecting massive changes feels realistic. I keep it simple, one application at night, and throw in a light, non‑comedogenic moisturizer if my skin gets a bit tight. It’s low‑key but works for me.
Kasey Mynatt
October 22, 2025 AT 03:23Whoa, that breakdown was fire! You managed to demystify the ribosomal inhibition while keeping it accessible-kudos! I’ve always been wary of mixing antibiotics with other actives, but your note on timing really clears the fog. The nuance between oxidative and protein synthesis pathways is something I wish more clinicians highlighted. Keep the science coming; it’s like a backstage pass to our skin’s battle front.
Edwin Pennock
October 23, 2025 AT 01:36Honestly, I think calling it “overpriced” misses the bigger picture-Clindamycin’s targeted action can actually prevent scarring, which cheaper options sometimes don’t. If you’re okay with a bit of dryness, the trade‑off might be worth it for the long‑term skin health.
Shriniwas Kumar
October 23, 2025 AT 23:50From an Indian dermatology standpoint, we often see patients with post‑adolescent acne who respond well to a combination of clindamycin gel plus a niacinamide serum, which helps mitigate hyperpigmentation that’s common in higher Fitzpatrick skin types. The synergy between the antibiotic’s antimicrobial effect and niacinamide’s barrier‑strengthening properties is supported by several regional studies. Moreover, advising patients to avoid sun exposure while on the regimen reduces the risk of post‑inflammatory hypermelanosis. This protocol aligns with both efficacy and cosmetic acceptability in our demographic.
Jennifer Haupt
October 24, 2025 AT 22:03While your combination sounds solid, I must challenge the blanket recommendation of niacinamide without addressing potential formulation incompatibilities-some gels can alter its pH stability, undermining efficacy. It would be more rigorous to suggest a specific pH‑balanced niacinamide product or to stagger application times to preserve each agent’s activity. Additionally, the claim about “regional studies” should be backed by citations; otherwise, the argument lacks scholarly weight. Let’s ensure we’re not just offering anecdotal guidance but evidence‑based protocols.
Bart Cheever
October 25, 2025 AT 20:16Jennifer, your insistence on citing sources is commendable yet somewhat pedantic; the referenced Indian studies are readily accessible via PubMed and provide sufficient validation for the regimen. Moreover, the pH concern, while technically accurate, is often mitigated by the buffering capacity of modern formulations, rendering the issue moot for most consumers. In short, the original suggestion remains practically sound.
kiran kumar
October 26, 2025 AT 17:30i think most of u miss the point that using antibiotics topically is just a band aid it doesn't solve the root cause and overuse will lead to super bugs we all gotta think long term
Brian Johnson
October 27, 2025 AT 15:43Brian here – you raise a valid concern about antibiotic stewardship. While topical clindamycin can be effective short‑term, rotating with benzoyl peroxide or a retinoid does help limit resistance. It’s a balance between immediate acne control and long‑term microbial health.
Shouvik Mukherjee
October 28, 2025 AT 13:56Adding to Brian’s point, patients can also incorporate a probiotic skincare line to support the skin microbiome while on antibiotics. This complementary approach may further diminish the risk of dysbiosis and maintain a healthier barrier.
Ben Hooper
October 29, 2025 AT 12:10Does anyone have data on how quickly resistance emerges with daily clindamycin use?
Marjory Beatriz Barbosa Honório
October 30, 2025 AT 10:23Great question, Ben! Studies suggest that bacterial resistance can start to appear as early as 8‑10 weeks of continuous use, especially without a benzoyl peroxide partner. That’s why many docs recommend a rotating schedule or combo therapy to keep the microbes on their toes.
G.Pritiranjan Das
October 31, 2025 AT 08:36Got it – so a 2‑month cycle with adjunctive BPO is a practical rule of thumb.