Autoimmune Disorder Medications: Understanding Immunosuppression Complications
 Jan, 17 2026
Jan, 17 2026
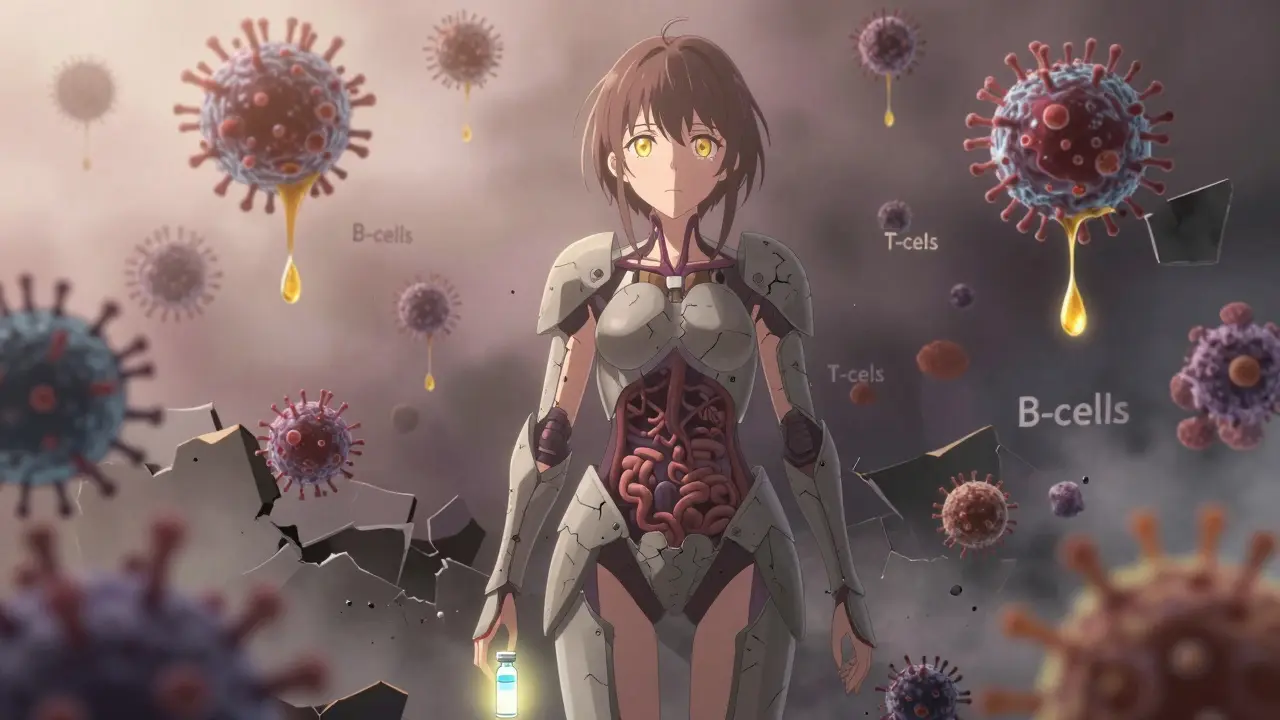
When you have an autoimmune disorder like rheumatoid arthritis, lupus, or Crohn’s disease, your immune system turns on your own body. Medications that suppress this overactive response can stop joint damage, skin flares, and gut inflammation. But every time you silence part of your immune system, you’re also lowering your body’s defenses. The trade-off isn’t just theoretical-it shows up in hospital visits, missed work, and life-altering infections.
What Happens When Your Immune System Is Turned Down
Immunosuppressive drugs don’t just calm inflammation-they shut down key parts of your body’s defense network. Think of your immune system like a security team. These medications don’t just disarm the guards who attack your joints or skin-they also turn off the ones watching for viruses, bacteria, and even early cancer cells. The most common drugs in this category fall into six groups. Corticosteroids like prednisone are fast-acting but come with broad, dose-dependent suppression. If you’re on more than 20 mg a day for over two weeks, your risk of serious infections like pneumonia or fungal infections spikes. Even after you stop taking them, your body stays vulnerable for weeks. Many patients don’t realize this window exists until they get sick. Biologics like adalimumab and rituximab target specific immune cells. That sounds better, right? But rituximab wipes out B-cells for up to six months after the last infusion. That means you can’t fight off common viruses like chickenpox or shingles, even if you’ve had them before. One patient on a rheumatology forum described getting shingles that lasted four months after a rituximab infusion-his doctor never warned him about the six-month risk window.The Hidden Dangers of Different Drug Classes
Not all immunosuppression is the same. Each drug class has its own fingerprint of risks.- Corticosteroids: Cause the widest suppression. Patients on long-term doses have 10-15% higher rates of opportunistic infections than those on biologics, even when disease control is equal.
- JAK inhibitors (tofacitinib, baricitinib): These oral pills are popular for convenience, but they carry unique dangers. They triple the risk of herpes zoster (shingles) compared to older drugs. They also raise the risk of blood clots-1.5 to 2 extra events per 1,000 patients each year. The FDA added a black box warning in 2021 after studies showed higher rates of heart attacks and strokes.
- Calcineurin inhibitors (cyclosporine, tacrolimus): These are tough on the kidneys. About one in three patients develops measurable kidney damage within two years. Regular blood tests are non-negotiable.
- mTOR inhibitors (sirolimus): These slow wound healing. In transplant patients, over 20% needed surgery for open wounds that wouldn’t close. If you’re on this drug and need dental work or surgery, plan ahead.
- IMDH inhibitors (azathioprine, mycophenolate): These can crash your bone marrow. Monthly blood counts aren’t optional-they catch low white blood cells before you get sick.
- Biologics: Rituximab stands out. It leaves patients unprotected for half a year. Hepatitis B can flare up silently. One in 50 people on rituximab reactivates it. That’s why blood tests for hepatitis B are required before starting.
Even methotrexate, often seen as the "safe" starter drug, isn’t risk-free. It raises infection risk by 1.2 times compared to the general population. But compared to biologics, it’s the least dangerous option for low-risk patients. Hydroxychloroquine, used for mild lupus or arthritis, barely affects immunity. Patient reviews on Drugs.com give it a 7.8 out of 10 for safety-far above biologics (6.2) and JAK inhibitors (5.9).
Why Vaccines Often Come Too Late
Vaccines are your best defense. But timing matters more than you think. If you’re about to start a B-cell depleting drug like rituximab, you need all your vaccines-flu, pneumonia, shingles, hepatitis B-at least four weeks before your first infusion. After the drug hits, your body can’t respond to vaccines for up to a year. That means if you wait until you’re already on treatment, the shots won’t work. A 2022 study found that 68% of serious infections in immunosuppressed patients could’ve been prevented with proper vaccination timing. Yet, a 2023 survey showed only 39% of patients on biologics had received the shingles vaccine before starting treatment. Many doctors still don’t prioritize this. One nurse with rheumatoid arthritis wrote on HealthUnlocked: "I’ve seen colleagues on JAK inhibitors get recurrent shingles despite vaccination-now I check my VZV titers every six months. No one told me to do that."
Who’s at the Highest Risk?
Not everyone on these drugs gets sick. Risk isn’t just about the drug-it’s about you.- Age over 65: Your immune system naturally weakens. Add immunosuppression, and your risk of pneumonia, sepsis, and cancer skyrockets.
- Smoking: Increases lung cancer risk by 1.34 times if you’re on a JAK inhibitor.
- Previous infections: If you’ve had TB, hepatitis B, or shingles before, those can come back.
- Diabetes or chronic lung disease: These conditions already strain your defenses. Immunosuppression makes them worse.
The CDC and American College of Rheumatology now classify patients into risk tiers-not just "immunosuppressed" or "not." High-risk patients (like those who’ve had rituximab in the last six months) need monthly infectious disease check-ins. Moderate-risk patients get quarterly blood work. Low-risk patients on hydroxychloroquine or low-dose methotrexate need far less monitoring.
The Real Cost of Complications
These aren’t just medical risks-they’re financial and emotional burdens. In 2023, immunosuppression-related infections accounted for 18% of hospitalizations among autoimmune patients in the U.S., costing $4.2 billion. Insurance companies noticed. Since January 2023, Medicare requires prior authorization for biologics and JAK inhibitors-only if you’ve shown you’ve been vaccinated, tested for hepatitis B, and documented infection prevention steps. Patient surveys tell the human side. Of 3,215 people surveyed by the Arthritis Foundation, 42% stopped their biologic because they were afraid of getting sick. 28% had been hospitalized for an infection during treatment. One Reddit user wrote: "I chose to live with joint pain instead of risking another pneumonia. I’m 42. I have two kids. I can’t afford to be out of commission for months."
What You Can Do Right Now
If you’re on or considering immunosuppressive therapy, here’s what actually works:- Get all vaccines at least 4 weeks before starting-especially shingles, pneumococcal, and hepatitis B.
- Ask for a baseline blood test for hepatitis B, TB, and immunoglobulin levels before treatment begins.
- Know your drug’s specific risk. If you’re on rituximab, ask about B-cell counts. If you’re on a JAK inhibitor, ask about blood clot symptoms-swelling in legs, chest pain, sudden shortness of breath.
- Monitor for fever, cough, or unusual fatigue. Don’t wait for it to get worse. Call your doctor at the first sign.
- Don’t skip blood tests. Monthly CBCs for azathioprine or mycophenolate aren’t bureaucracy-they’re early warnings.
- Ask about alternatives. If you’re on high-dose prednisone, is there a lower-dose steroid or non-immunosuppressive option? Hydroxychloroquine is safer for mild cases.
There’s no perfect drug. But there’s a smarter way to use them. The biggest mistake isn’t taking the medication-it’s assuming all immunosuppression is the same. Your treatment plan should be as personalized as your fingerprint.
What’s Changing in 2026
The field is moving fast. The NIH launched a $28 million project in early 2023 to find biomarkers that predict who’s most likely to get sick. Early results suggest analyzing specific T-cell subsets could let doctors tailor monitoring-some patients might need weekly checks, others only annual ones. Newer drugs like upadacitinib (Rinvoq) come with black box warnings and mandatory vaccination protocols. The FDA now requires all prescribers of JAK inhibitors to complete risk education. And AI tools are being tested to predict infection risk from your EHR-Mayo Clinic’s prototype cut serious infections by 22% in a pilot study. But the biggest shift? Doctors are finally moving past "you’re immunosuppressed" and into "here’s exactly what’s suppressed, for how long, and what that means for you."By 2030, over a million Americans over 65 will be on biologics. Without smarter, personalized approaches, we’ll see a surge in preventable deaths. The goal isn’t to avoid these drugs-it’s to use them with eyes wide open.
Can I still get vaccinated while on immunosuppressive drugs?
Yes, but timing is everything. Live vaccines (like MMR, shingles, nasal flu) are dangerous if your immune system is suppressed. Inactivated vaccines (flu shot, pneumonia, COVID-19, hepatitis B) are safe-but only if given at least 4 weeks before starting drugs like rituximab or cyclosporine. After starting, vaccines often don’t work well. Check with your rheumatologist before scheduling any shots.
How do I know if my immunosuppressive drug is too risky for me?
There’s no one-size-fits-all answer. Your risk depends on your age, other health conditions, smoking status, and which drug you’re on. If you’re over 65, smoke, or have diabetes, JAK inhibitors and high-dose steroids carry higher risks. If you’ve had hepatitis B or TB before, certain biologics can reactivate them. Ask your doctor for a risk stratification-many clinics now use tools that categorize you as low, moderate, or high risk based on your specific regimen.
Are there safer alternatives to biologics and JAK inhibitors?
Yes, depending on your condition. For mild rheumatoid arthritis or lupus, hydroxychloroquine has minimal immunosuppression and is among the safest options. Low-dose methotrexate (25 mg/week or less) increases infection risk only slightly-1.2 times higher than the general population. Sulfasalazine is another option for gut-related autoimmune conditions with lower systemic risk. Talk to your doctor about whether your disease severity justifies a stronger drug.
Why do I need monthly blood tests if I feel fine?
Many complications don’t cause symptoms until it’s too late. Azathioprine and mycophenolate can silently lower your white blood cell count. You might feel fine, but without enough white cells, a simple cold can turn into pneumonia. Monthly complete blood counts catch this early. Skipping them is like driving without checking your oil light-eventually, something breaks.
Can immunosuppressive drugs cause cancer?
Yes, but the risk is small and tied to specific drugs and patients. JAK inhibitors slightly increase the risk of lymphoma and lung cancer, especially in smokers over 65. The FDA found a 1.44-fold higher lymphoma risk with these drugs. Biologics carry a small risk of skin cancer and lymphoma, but the absolute numbers are low-about 0.5 to 1 case per 1,000 patients per year. Regular skin checks and avoiding smoking reduce this risk significantly. The benefit of controlling severe autoimmune disease often outweighs the small cancer risk.
What should I do if I get sick while on these medications?
Don’t wait. If you have a fever over 100.4°F, unexplained fatigue, a new cough, or a rash that spreads quickly, contact your rheumatologist immediately. Don’t assume it’s just a cold. Many infections in immunosuppressed patients progress fast. Your doctor may need to pause your medication, start antibiotics or antivirals, or run urgent blood tests. Early action saves lives.

Jake Moore
January 18, 2026 AT 13:07Just wanted to say this post is a godsend. I was on rituximab for lupus and had no idea the B-cell suppression lasted six months. My doctor never mentioned it. Got shingles six months post-infusion and was in hell for three months. If you're on any biologic, ask for a B-cell count before and after. It's not optional.
Joni O
January 19, 2026 AT 17:30Thank you for writing this. I’m on low-dose methotrexate and felt guilty for not being "serious enough" about my RA. Turns out I’m actually in the low-risk tier? I’m gonna print this out and show my rheumatologist. Also, hydroxychloroquine for mild lupus is a total lifesaver-no more scary blood tests, no more infections. Just a little fatigue and my skin feels better than ever.
Andrew Qu
January 20, 2026 AT 19:44Monthly CBCs for azathioprine aren’t bureaucracy-they’re your early warning system. I skipped mine for two months because I felt fine. Ended up with neutropenia and a UTI that turned into sepsis. Hospital for 11 days. Don’t be me. Get the bloodwork. Even if you feel 100%. Your body doesn’t lie.
kenneth pillet
January 21, 2026 AT 07:30Got the shingles vaccine before starting JAK inhibitor. Still got it. Six months later. Now I check VZV titers every six months. No one told me to. Just saying.
Selina Warren
January 22, 2026 AT 17:40This isn’t medicine. It’s Russian roulette with your immune system. They give you a drug that turns off your body’s alarm system, then act shocked when you get sick. And don’t get me started on the insurance companies now requiring prior auth for vaccines you should’ve gotten *before* the drug. Who’s really in charge here? The doctor? The FDA? Or the profit margins?
Emma #########
January 23, 2026 AT 14:26I’m 58, on hydroxychloroquine for SLE. I’ve been on it 12 years. Never had a serious infection. I get my flu shot every fall. I don’t smoke. I sleep 8 hours. I don’t stress about it. This post made me feel seen. You don’t have to be scared. You just have to be smart.
Eric Gebeke
January 23, 2026 AT 21:10Wow. Another one of those posts where someone pretends they discovered the wheel. Of course immunosuppressants suppress immunity. That’s why they’re called immunosuppressants. Did you really think your body would just magically know to keep fighting infections while also calming your immune system? This is basic pharmacology 101. And yet here we are, people acting like this is some groundbreaking revelation. You didn’t need a 3,000-word essay to figure this out. Just read the damn drug leaflet.
Jay Clarke
January 24, 2026 AT 06:33So let me get this straight-you’re telling me the system that’s supposed to save me is also trying to kill me? And the doctors are just shrugging? I’m 39. I have two kids. I don’t want to be a statistic. I’m done with biologics. I’m switching to turmeric and prayer. At least then I’m not poisoning myself with corporate science.
Nishant Sonuley
January 25, 2026 AT 17:00Look, I get it. You’re scared. I’m from India, and here, even basic healthcare access is a battle. But let’s not pretend this is unique to the US. Every country has this tension-between controlling disease and preserving life. The real issue isn’t the drugs. It’s that we treat autoimmune conditions like they’re a checklist, not a living, breathing human being with a history, fears, and a family. The system needs to stop being a factory and start being a sanctuary. And yes, that means more time, more listening, more patience. But isn’t that what medicine was supposed to be?
Andrew McLarren
January 27, 2026 AT 10:06While the clinical data presented is both comprehensive and compelling, I would respectfully suggest that the emotional weight of patient testimonials-while valuable-may inadvertently introduce selection bias into the risk-perception framework. A more rigorous approach would involve stratified longitudinal cohort analysis, controlling for socioeconomic variables, medication adherence, and baseline comorbidity burden. The current narrative, though persuasive, risks oversimplifying a multivariate clinical challenge.
Andrew Short
January 27, 2026 AT 21:55Let’s be real-this whole thing is a scam. Big Pharma knows these drugs cause cancer and infections. They just don’t care because people are too scared to stop taking them. The FDA? Paid off. The doctors? Too busy to care. And now they’re forcing you to get vaccinated before they’ll give you the poison that’s going to make you sick anyway. It’s not medicine. It’s extortion with a stethoscope.
christian Espinola
January 28, 2026 AT 03:41Typo in the JAK inhibitor section: "1.5 to 2 extra events per 1,000 patients each year"-should be "per 1,000 patient-years." Also, the CDC doesn’t classify risk tiers. The ACR does. And the NIH project is $28 million over five years, not "launched in early 2023." This post is full of sloppy details. If you’re going to write something this technical, at least fact-check it.
Ryan Otto
January 28, 2026 AT 19:06Let me ask you something. If your immune system is being deliberately disabled by pharmaceutical agents, and you’re being told to get vaccinated before the suppression begins-why wasn’t this protocol standard since the 1990s? Why is it only being enforced now, after tens of thousands have been hospitalized? Why are there no long-term studies on the cumulative effect of multiple immunosuppressants over decades? And why, pray tell, is the FDA only now requiring prescriber education? Coincidence? Or is this the slow reveal of a systemic failure that was always known? I’m not paranoid. I’m just reading the receipts.