Adrenal Insufficiency from Corticosteroid Withdrawal: How to Recognize and Manage It
 Jan, 23 2026
Jan, 23 2026
Adrenal Insufficiency Taper Calculator
How to Use This Tool
This calculator helps determine a safe tapering schedule based on your steroid therapy. Always consult your doctor before adjusting medications.
EMERGENCY WARNING
Do not stop steroids abruptly. If you experience any of these symptoms:
- Severe fatigue
- Nausea/vomiting
- Low blood pressure
- Dizziness when standing
- Confusion
You need emergency hydrocortisone immediately. Call 911 or go to emergency room.
Stopping corticosteroids like prednisone or dexamethasone suddenly can trigger a medical emergency you might never see coming. Even if you’ve only taken them for a few weeks, your body may not be able to make enough cortisol - the hormone that keeps you alive under stress. This isn’t just fatigue or a bad day. It’s adrenal insufficiency, and it can kill you if no one recognizes the signs.
Why Your Body Stops Making Cortisol
When you take corticosteroids for weeks or months, your brain gets the message: "We’ve got plenty of cortisol already." So it shuts down the signals to your adrenal glands. Over time, those glands shrink and forget how to produce cortisol on their own. This is called hypothalamic-pituitary-adrenal axis (HPAA) suppression. It’s not a side effect - it’s a physiological rewrite of your body’s natural rhythm. You don’t need to be on high doses for this to happen. Studies show even 5 mg of prednisone daily for more than four weeks can cause adrenal suppression. And it’s not just long-term users. A 2023 study in Endocrine Abstracts found that 30% of patients who took steroids for under four weeks still had suppressed cortisol levels after stopping. The myth that "short-term use is safe" is dangerous and outdated.What Happens When You Stop Too Fast
The moment you stop taking your steroid, your body is left without its artificial cortisol supply. But your adrenals haven’t woken up yet. That’s when symptoms start - usually within 24 to 72 hours. Early signs are easy to miss because they look like the flu, depression, or just being tired:- Severe fatigue (85% of cases)
- Loss of appetite and unexplained weight loss (72%)
- Nausea, vomiting, or stomach pain (68%)
- Muscle weakness (65%)
- Low mood, irritability, or brain fog (58%)
How Doctors Diagnose It
If you’ve been on steroids and now feel awful, your doctor should test for adrenal insufficiency. The standard test is the ACTH stimulation test. You get an injection of synthetic ACTH, then your blood is drawn an hour later to see if your adrenals respond by making cortisol. A level below 18 μg/dL after the test means your adrenals aren’t working. But there’s a simpler clue: the morning cortisol level. If your blood cortisol is under 5 μg/dL 24 hours after your last steroid dose, you’re at high risk for withdrawal symptoms. If it’s above 10 μg/dL, you’re likely fine. This isn’t perfect, but it’s a quick, cheap way to spot trouble before you end up in the ER. There’s also a tricky gray area called glucocorticoid withdrawal syndrome. It mimics adrenal insufficiency - muscle aches, joint pain, fatigue - but cortisol levels may be normal. The difference? Withdrawal syndrome doesn’t cause low blood pressure or electrolyte imbalances. Still, it’s painful and real. Many patients are told it’s "just psychological," but the symptoms are physical and often last weeks.
How to Taper Safely
The only way to avoid adrenal insufficiency is to taper slowly. But there’s no one-size-fits-all schedule. It depends on how long you were on steroids, your dose, your health, and how your body responds. The American College of Physicians recommends this general approach:- For doses over 20 mg prednisone daily: Reduce by 2.5-5 mg every 3-7 days.
- For doses between 5-20 mg: Reduce by 1-2.5 mg every 1-2 weeks.
- For anyone on steroids longer than 6 months: Slow down even more - sometimes reducing by 0.5-1 mg every 2-4 weeks.
What to Do in an Emergency
If you’re in adrenal crisis - low blood pressure, confusion, vomiting, fainting - you need hydrocortisone now. Not tomorrow. Not when you get to the hospital. You need it in the next 30 minutes. In the ER, treatment is straightforward: a 100 mg IV bolus, followed by 200 mg infused over 24 hours. Blood pressure usually improves within an hour. If you’re at risk, your doctor should give you an emergency injection kit - usually 100 mg of hydrocortisone in a syringe. Learn how to use it. Keep it with you. Tell your family how to use it too. Wear a medical alert bracelet that says "Adrenal Insufficiency" and lists your steroid history. Many patients who survive crisis say their bracelet saved their life.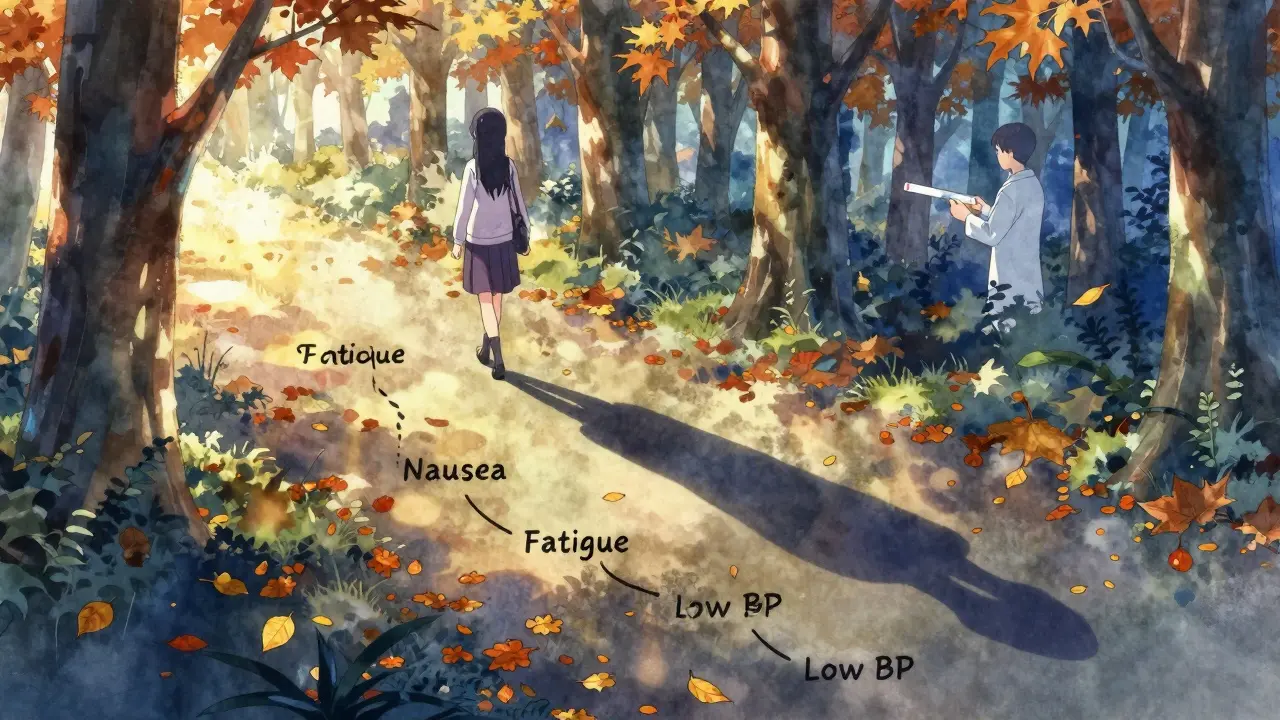
Who’s at Risk - And Who’s Overlooked
You might think only people on high-dose steroids for years are at risk. That’s wrong. People on low doses for asthma, eczema, or even short-term COVID-19 treatment are now showing up in ERs with adrenal crisis. A 2023 study found that 1 in 5 adrenal crisis cases came from patients who took steroids for less than 8 weeks. The real danger? Doctors don’t ask. Patients don’t know. A 2024 survey of 85 patients found that 68% had their symptoms dismissed as something else - viral illness, depression, stress. One man lost 20 pounds and couldn’t walk for six weeks before anyone tested his cortisol. He had been on 10 mg of prednisone for six weeks after pneumonia. Even after you stop, you’re not out of the woods. Your body can take months to recover. During that time, any major stress - surgery, infection, trauma - can trigger crisis. You may need stress-dose steroids again. Your doctor should give you a written plan for what to do if you get sick.What You Can Do Today
If you’re currently taking corticosteroids:- Ask your doctor: "Am I at risk for adrenal insufficiency?"
- Get a written tapering plan - don’t rely on memory.
- Request an emergency hydrocortisone injection kit.
- Get a medical alert bracelet.
- Teach someone close to you how to give the injection.
- Keep your medication guide - all systemic steroids now come with one by FDA rule since 2021.
- Don’t wait for symptoms to get worse.
- Go to urgent care or the ER - say: "I stopped steroids recently and think I might have adrenal insufficiency."
- Bring your medication history with you.
What’s Changing in 2026
New tools are coming. Point-of-care cortisol tests - devices that give results in 15 minutes - are in clinical trials and could soon be in doctors’ offices. AI systems are already analyzing electronic records to predict who’s at risk with 92% accuracy. Genetic testing may soon tell us who recovers slowly after steroids. But the biggest change is awareness. The Endocrine Society’s 2024 guidelines now require all providers to educate patients at the start of steroid therapy. The American Medical Association added adrenal crisis recognition to its mandatory continuing education list. And in 28 European countries, patients now get a standardized alert card with every steroid prescription. The goal? Cut adrenal crisis deaths by 30% by 2030. That won’t happen with better drugs. It’ll happen because patients and doctors finally understand: stopping steroids isn’t just about quitting a pill. It’s about reawakening your body’s survival system.Can adrenal insufficiency happen after just a few weeks of steroids?
Yes. Even short-term use - as little as 4 weeks at doses above 5 mg of prednisone daily - can suppress your adrenal glands. A 2023 study in Endocrine Abstracts found that 30% of patients who took steroids for under 4 weeks still had low cortisol levels after stopping. The old belief that only long-term users are at risk is outdated and dangerous.
What are the first signs of adrenal insufficiency after stopping steroids?
The earliest signs are fatigue, loss of appetite, nausea, muscle weakness, and low mood. These often appear 24-72 hours after the last dose and are easily mistaken for the flu, depression, or burnout. If you’ve recently stopped steroids and feel unusually tired or sick, don’t wait - get your cortisol checked.
Is adrenal crisis always obvious?
No. Many patients are misdiagnosed for weeks. Symptoms like vomiting, low blood pressure, and confusion are often blamed on infections, food poisoning, or anxiety. One patient spent six weeks being treated for a UTI before being diagnosed with adrenal crisis. If you’re on steroids and feel worse after stopping, always consider adrenal insufficiency as a possibility.
Do I need an emergency injection if I’m tapering slowly?
Yes. Even with a slow taper, your adrenal glands may not recover fast enough if you get sick, injured, or stressed. The Endocrine Society recommends all patients on long-term steroids carry an emergency hydrocortisone injection. It’s not a backup - it’s a lifeline. Use it if you can’t keep food down, feel faint, or have severe vomiting.
How long does it take for adrenal glands to recover after stopping steroids?
Recovery time varies. For some, it takes weeks. For others, especially those on high doses or long-term therapy, it can take 6 to 12 months or longer. There’s no way to predict exactly. Until your cortisol levels normalize, you’re still at risk for adrenal crisis during physical stress. Your doctor should monitor you with blood tests during recovery.

Juan Reibelo
January 23, 2026 AT 20:54Wow. This is one of those posts that makes you realize how little we’re taught about our own bodies.
My uncle died from this after a short prednisone course for asthma. They thought it was a heart issue.
He was 52. No warning. No bracelet. No emergency kit.
Doctors never asked if he’d been on steroids. No one ever told him to taper.
It’s not just medical negligence-it’s systemic ignorance.
I’m sharing this with every family member who’s ever been prescribed corticosteroids.
Someone needs to make this mandatory in every prescription packet.
Not optional. Not a footnote. A red flag.
Dolores Rider
January 24, 2026 AT 17:33they’ve been hiding this for decades lol
big pharma doesn’t want you to know you can die from quitting a pill
they make billions off the emergency visits and long-term hormone replacements
you think this is medicine? it’s a profit loop
they’ll sell you the injection kit AND the follow-up blood tests AND the ‘stress dose’ meds
and still charge you for the ‘misdiagnosis’
the bracelet? that’s just a bandaid on a hemorrhage
they want you scared enough to keep coming back
but not scared enough to sue them
watch this get buried under 10k comments about ‘just take your meds’
it’s always the same 😔
John McGuirk
January 25, 2026 AT 02:03you ever notice how the FDA only started requiring those medication guides in 2021?
right after the lawsuits started piling up
and now suddenly everyone’s like ‘oh wow this is dangerous’
but they knew for 30 years
the endocrine society’s 2024 guidelines? that’s just damage control
they’re not trying to save lives
they’re trying to avoid being sued
and don’t even get me started on those ‘point-of-care cortisol tests’
that’s just the next billing code waiting to happen
they’ll charge $400 for a 15-minute test and call it innovation
same old game
same old lies
you’re not getting better
you’re just getting billed
Michael Camilleri
January 26, 2026 AT 19:35people think medicine is about healing
it’s not
it’s about control
you take the pill
you follow the schedule
you don’t question the system
but when you finally try to break free
they act like you’re the problem
not the drug
not the lack of education
not the fact that no one warned you
you’re not weak
you’re not lazy
you’re not imagining the fatigue
you’re just a pawn in a system that profits from your dependence
and now they want you to wear a bracelet like a criminal
so they can say ‘we told you’
but they didn’t tell you
they just handed you the pill and walked away
that’s not medicine
that’s abandonment with a stethoscope
Darren Links
January 28, 2026 AT 02:41why do Americans always think everything’s a conspiracy?
Canada’s been doing this right for years
we have mandatory patient handouts
we have standardized tapering protocols
we have ERs trained to ask ‘steroid history?’
it’s not magic
it’s just basic accountability
your system’s broken because you let corporations write your healthcare rules
not because doctors are evil
because they’re overworked and under-resourced
and yeah maybe the system’s flawed
but blaming ‘big pharma’ won’t fix it
fixing it requires policy
not paranoia
Kevin Waters
January 29, 2026 AT 08:34I’m an ER nurse and I’ve seen this too many times.
Patients come in pale, shaking, confused - and they say ‘I just stopped my prednisone’ and everyone thinks it’s anxiety.
One guy came in with a 104 fever and vomiting - we ran every test, nothing.
Then his wife remembered he’d been on 20mg for 8 weeks.
We gave him 100mg IV hydrocortisone.
He sat up 20 minutes later and asked for a sandwich.
That’s it. That’s the whole story.
If you’re on steroids - get the kit. Wear the bracelet. Tell your family.
It’s not dramatic. It’s just smart.
And if you’re a doctor - stop assuming short-term means safe.
We’ve got the data. We’ve got the tools.
Let’s stop pretending this is rare.
It’s not.
It’s preventable.
And it’s happening every day.
Sawyer Vitela
January 31, 2026 AT 07:5830% of short-term users have suppressed cortisol? That’s the stat.
Everything else is noise.
Stop tapering too fast.
Get tested.
Carry the shot.
Done.
Tiffany Wagner
February 2, 2026 AT 07:52i was on prednisone for 6 weeks for a bad allergic reaction
stopped it cold turkey because my doctor said it was fine
then i spent 3 weeks feeling like i was dying
no one believed me
i thought i was losing my mind
finally went to a new doctor and she checked my cortisol
it was below 3
she gave me a tiny dose to restart and we tapered slowly
it took 4 months to feel normal again
no one warned me
no one asked
please just tell people
it’s not in your head
it’s real
and you’re not alone
Chloe Hadland
February 3, 2026 AT 13:04thank you for writing this
i’ve been through it
and honestly? the hardest part wasn’t the symptoms
it was the guilt
feeling like i should’ve known
like i failed because i didn’t ask the right questions
but you didn’t fail
the system did
so thank you for making this so clear
now i’m telling everyone i know
because no one else should feel as lost as i did